Articles
- Page Path
- HOME > J Korean Acad Community Health Nurs > Volume 33(4); 2022 > Article
- Original Article Factors Associated with Depression in Older Adults Living Alone during the COVID-19 Pandemic
- Eun Hye Hong, Kyung Hee Lee*
-
DOI: https://doi.org/10.12799/jkachn.2022.33.4.418
Published online: December 31, 2022

2Associate Professor, College of Nursing · Mo-Im Kim Nursing Research Institute, Yonsei University, Seoul, Korea

-
*Corresponding email:
kyungheelee@yuhs.ac
- 1,108 Views
- 38 Download
- 2 Crossref
- 0 Scopus
Abstract
Purpose
The aims of this study were to examine the rate of depression among older adults living alone and to identify factors associated with depression in older adults living alone during the COVID-19 pandemic.
Methods: A secondary data analysis was performed using data from the 2020 Korea Community Health Survey. The study participants were 18,824 older adults aged 65 years and over living alone. The data of the complex sample design was analyzed with consideration for weights, stratification, and clustering. Complex sample multiple logistic regression was conducted to identify factors associated with depression in older adults living alone during the COVID-19 pandemic.
Results: The results showed that the rate of depression in older adults living alone was 6.3%. Older adults living alone with decreased physical activity, decreased hours of sleep, and an increased or similar frequency of meeting with friends or neighbors were found to be more likely to have depression. In terms of factors related to the practice of COVID-19 infection prevention and control rules, not disinfecting regularly and not wearing a mask indoors were related to depression.
For health-related factors, fair or poor self-rated health status, not having breakfast every day, and feeling stressed were related to depression.
Conclusion: It is recommended to develop tailored interventions to prevent depression among older adults living alone by considering the factors related to their depression during the COVID-19 pandemic.
| J Korean Acad Community Health Nurs. 2022 Dec;33(4):418-431. English. Published online Dec 30, 2022. https://doi.org/10.12799/jkachn.2022.33.4.418 | |
| © 2022 Korean Academy of Community Health Nursing | |
Eun Hye Hong ,1
and Kyung Hee Lee ,1
and Kyung Hee Lee 2 2
| |
|
1Graduate Student, College of Nursing, Yonsei University, Seoul, Korea. | |
|
2Associate Professor, College of Nursing · Mo-Im Kim Nursing Research Institute, Yonsei University, Seoul, Korea. | |
Corresponding author: Lee, Kyung Hee. College of Nursing, Yonsei University, 50-1 Yonsei-ro, Seodaemun-gu, Seoul 03722, Korea. Tel: +82-2-2228-3321, Fax: +82-2-2227-8303, | |
| Received June 29, 2022; Revised November 28, 2022; Accepted November 29, 2022. | |
|
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by- | |
|
Abstract
| |
|
Purpose
The aims of this study were to examine the rate of depression among older adults living alone and to identify factors associated with depression in older adults living alone during the COVID-19 pandemic.
Methods
A secondary data analysis was performed using data from the 2020 Korea Community Health Survey. The study participants were 18,824 older adults aged 65 years and over living alone. The data of the complex sample design was analyzed with consideration for weights, stratification, and clustering. Complex sample multiple logistic regression was conducted to identify factors associated with depression in older adults living alone during the COVID-19 pandemic.
Results
The results showed that the rate of depression in older adults living alone was 6.3%. Older adults living alone with decreased physical activity, decreased hours of sleep, and an increased or similar frequency of meeting with friends or neighbors were found to be more likely to have depression. In terms of factors related to the practice of COVID-19 infection prevention and control rules, not disinfecting regularly and not wearing a mask indoors were related to depression. For health-related factors, fair or poor self-rated health status, not having breakfast every day, and feeling stressed were related to depression.
Conclusion
It is recommended to develop tailored interventions to prevent depression among older adults living alone by considering the factors related to their depression during the COVID-19 pandemic. |
|
Keywords:
Aged; COVID-19; Depression; Pandemics
|
|
|
INTRODUCTION
|
1. Background
The cases of the novel coronavirus disease (henceforth COVID-19) were first reported in Wuhan, China in December, 2019, and as this infectious disease gradually spread across the world, the World Health Organization (WHO) declared the novel coronavirus disease (COVID-19) outbreak a global pandemic on March 11, 2020 [1]. As of the end of September, 2022, the total number of confirmed cases of COVID-19 globally has exceeded 612.23 million, and 6.51 million of them died from COVID-19 worldwide [2]. In Korea, as of the end of September, 2022, the total number of confirmed cases of COVID-19 has exceeded 24.63 million, the cumulative number of deaths from COVID-19 is 28,246, and older adults aged 60 or older account for 93.6% of the total deaths from COVID-19 [3].
As the spread of COVID-19 and social distancing as a major preventive measure have continued for three years, prolonged pandemic and social distancing have led to an increase in the number of people suffering from depression throughout the society. According to the COVID-19 National Mental Health Survey First Quarter 2021, the proportion of the group at risk for depression is 22.8%, and this figure represents the percentage increased by about 6 times, compared to 3.8% in 2018 before the COVID-19 pandemic [4]. Briggs et al. [5] also reported that the proportion of the group at risk for depression among older adults residing in Ireland has more than doubled after the outbreak of COVID-19 from 7.2% in 2016 and 2018 to 19.8% in 2020. In particular, among older adults living alone, the proportion of the group at risk for depression has increased to 26.1% in 2020, compared to 10.2% in 2016 and 11.2% in 2018 before the COVID-19 pandemic, showing a considerable increase in the prevalence rate of depression among older adults living alone during the COVID-19 pandemic [5]. Therefore, there is a need to take measures for the prevention and management of depression due to COVID-19 and provide support for the group at risk for depression.
In the COVID-19 pandemic situation, the spread of COVID-19 infections and social distancing measures can act as risk factors for depression in older adults. Older adults are a high-risk group for COVID-19 infections, and as older adults stay at home to avoid COVID-19 infections, it results in a reduction in their physical activity, which increases the level of depression in older adults [6]. In addition, the COVID-19 pandemic was reported to cause poor sleep quality and changes in sleep hours in some older adults [6]. Moreover, restrictions on going out to public places and participation in social activities due to social distancing measures may have a negative effect on the emotional health of older adults [6]. In addition, with the spread of COVID-19 infections, the levels of fear and the psychological impact due to COVID-19 were reported to be higher in older adults vulnerable to coronavirus infections than in other age groups [7], and they were reported to affect depression in older adults [8]. A higher level of the psychological impact due to COVID-19 has been shown to be associated with a higher level of the practice of COVID-19 infection prevention and control rules [7], and it has been reported that the practice of COVID-19 infection prevention and control rules may affect depression in older adults [9]. Therefore, to understand depression in older adults, it is necessary to examine risk factors for depression due to the COVID-19 pandemic.
In particular, the COVID-19 pandemic may have a significant impact on depression in older adults living alone. This study was conducted using data from the 2020 Korea Community Health Survey. This survey was carried out from August to October, 2020, when the social distancing level was elevated to level 2 nationwide in Korea, and level-2 social distancing was implemented for 7 weeks. The implementation of level-2 social distancing included measures such as prohibition of unnecessary going out, gatherings and rallies, closing social welfare facilities, and prohibition of face-to-face worship services at churches [10]. These COVID-19 social distancing measures may cause a greater sense of social isolation in older adults living alone who get social support or emotional support through the use of senior centers or senior welfare facilities or participation in social activities than in older adults living with their families, and disconnection of social networks and increased social isolation may result in the increased prevalence rate of depression in older adults living alone [11]. In addition, in previous studies conducted before the outbreak of the COVID-19 pandemic, the prevalence rate of depression was found to be higher in older adults living alone than in those living together with their families [12, 13]. Likewise, the prevalence rate of depression was found to be higher in older adults living alone than in older adults with cohabitants during the COVID-19 pandemic [5]. Therefore, since older adults living alone are a vulnerable group that cannot share their feelings and experience about COVID-19 or receive direct care from their families, the rate of depression is likely to be higher in older adults living along than in other population groups. For this reason, it is important not only for individuals but also for the society to identify the influencing factors for depression.
Depression in older adults living alone has been reported to be related to sociodemographic factors, such as age [14], sex, educational level [13, 14], status of the basic livelihood security recipient (henceforth, basic living recipient) [13], economic status [14], and health-related factors such as subjective health status [14], chronic disease [12, 13, 14], and stress [12]. Although a number of studies have been so far conducted on depression in older adults living alone, there has been a lack of studies to investigate risk factors for depression in older adults living alone through a comprehensive and integrated analysis of risk factors for depression arising during the COVID-19 pandemic, so there is a need to examine such risk factors using a large data representative of the national population. Therefore, this study attempted to investigate factors associated with depression in older adults living alone during the COVID-19 pandemic by using data from the 2020 Korea Community Health Survey with the aim of presenting basic data for interventions for the prevention and appropriate management of depression in older adults living alone in the future.
2. Purpose
This study aimed to examine factors associated with depression among older adults living alone during the COVID-19 pandemic, and the specific objectives of this study are as follows:
• To investigate the rate of depression, factors related to changes in daily life due to COVID-19, factors related to the practice of COVID-19 infection prevention and control rules, factors related to the psychological impact due to COVID-19, sociodemographic factors, and health-related factors among older adults living alone;
• To examine differences in depression depending on factors related to changes in daily life due to COVID-19, factors related to the practice of COVID-19 infection prevention and control rules, factors related to the psychological impact due to COVID-19, sociodemographic factors, and health-related factors among older adults living alone;
• To identify factors associated with depression among older adults living alone during the COVID-19 pandemic.
|
METHODS
|
1. Study Design
This study is a secondary data analysis using data from the 2020 Korea Community Health Survey to investigate factors associated with depression in older adults living along during the COVID-19 pandemic.
2. Participants
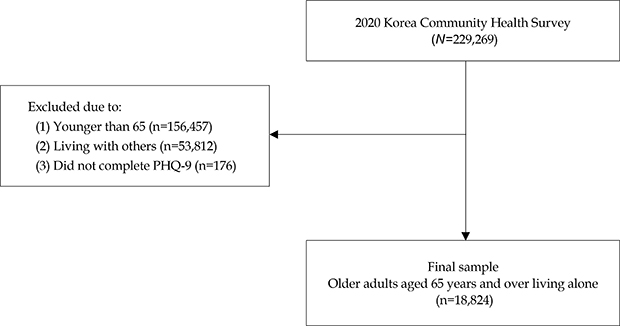
This study was conducted using data from the 2020 Korea Community Health Survey provided by the Korea Disease Control and Prevention Agency. The participants of the survey are adults aged 19 or older who were the household members of the sample households at the time of the survey. They were selected by a complex sampling design that initially extracts sample points based on the number of households by housing type in the administrative divisions of tong/ban/li by probability proportional to size (PPS) systematic sampling, and secondarily extracts sample households by systematic sampling. The 2020 Korea Community Health Survey was conducted from August 16 to October 31, 2020, and trained interviewers personally visited the selected sample households and conducted a one-to-one interview survey by the computer assisted personal interviewing (CAPI) method using a laptop. The contents of the survey included the basic demographic information of participants, health status, the presence of diseases, the use of medical services, the sociophysical environment, educational level, economic activities, the experience of symptoms related to COVID-19, the practice of personal rules for infection prevention and control, the practice of social distancing, changes in daily life, and psychological concerns [15]. The participants of this study were older adults aged 65 or older living alone who participated in the 2020 Korea Community Health Survey. Among a total of 229,269 respondents of the 2020 Korea Community Health Survey, only 18,824 older adults aged 65 or older living alone were included in this study by sequentially excluding respondents aged under 65 years (n=156,457), those with one or more cohabitants (n=53,812), and those who did not respond to any of the 9 items of a Korean version of the Patient Health Questionnaire-9 (PHQ-9) (n=176) (Appendix 1).
3. Measures
1) Depression
In this study, depression is the dependent variable, and it was measured using a Korean version of the PHQ-9, which is a self-report depression scale with 9 items [16]. The PHQ-9 is composed of 9 items on the loss of interest in work, depression, sleep disorder, fatigue, appetite, a feeling of unhappiness, a decrease in concentration, anxiety behavior, and self-depreciation. Each item is measured on a 4-point Likert scale, and higher scores indicate higher levels of depression. The total scores ranged from 0 to 27 points. Based on the cut-off score of 10 points, scores of ≤9 points were classified into the non-depression group and scores of ≥10 points were classified into the depression group [17]. The Cronbach's α value of the Korean version of PHQ-9 was reported as .85 by the developer [16], and the Cronbach's α value was .82 in this study.
2) Factors related to changes in daily life due to COVID-19
Factors related to changes in daily life due to COVID-19 were examined using questions on what changes occurred in daily life during the COVID-19 pandemic compared to before the COVID-19 pandemic. In this study, factors related to changes in daily life were a total of 3 items about physical activity, sleep hours, and meeting with friends or neighbors. The 2020 Korea Community Health Survey examined changes in the following 8 factors: physical activity, sleep hours, consumption of instant foods or soft drinks, consumption of delivery foods, drinking, smoking, meeting with friends or neighbors, and the use of public transportation. However, some items had a very high rate of missing responses, and the rate of missing responses was 62.2% for consumption of instant foods or soft drinks, 82.5% for consumption of delivery foods, 71.6% for drinking, 88.9% for smoking, and 27.7% for the use of public transportation. In this study, these factors were excluded from the analysis of factors related to changes in daily life due to a very high rate of missing responses. Meanwhile, 'changes in eating habits' (consumption of instant foods or soft drinks, consumption of delivery foods) may overlap with 'frequency of having breakfast during a week' among health-related factors, and changes in drinking and changes in smoking may overlap with 'drinking' and 'smoking' variables among health-related factors, so they were included only in health-related factors. Changes in physical activity, sleep hours, and meeting with friends or neighbors were dichotomously categorized into 'Increased or similar' and 'Decreased'.
3) Factors related to the practice of COVID-19 infection prevention and control rules
Based on the contents of the personal practice guidelines on COVID-19 infection prevention and control of the 4th edition of the basic guidelines on social distancing in daily life of the Central Disaster and Safety Countermeasures Headquarters (CDSCHQ) [18], factors related to the practice of COVID-19 infection prevention and control rules were selected as follows: performing regular ventilation, performing regular disinfection, wearing a mask indoors, wearing a mask outdoors, and keeping in touch with close people (non-face-to-face contact) despite not meeting together. These factors were dichotomously categorized into 'Yes' and 'No'.
4) Factors related to the psychological impact due to COVID-19
The factors related to the psychological impact due to COVID-19 examined in this study were as follows: concerns about COVID-19 infection, concerns about death from COVID-19 infection, concerns about criticism from others due to COVID-19 infection, concerns about economic damage due to COVID-19, and the number of people who can help during quarantine treatment or self-quarantine. These four factors about concerns due to COVID-19 were measured on a 5-point Likert scale (Strongly agree, Agree, Neutral, Disagree, Strongly disagree) in the raw data, but these factors were categorized into Yes (Strongly agree/Agree), Average (Neutral), and No (Disagree/Strongly disagree) in this study. For the number of people who can help during quarantine treatment or the self-quarantine period, this factor was dichotomously categorized into 'No one' or 'One or more persons'.
5) Sociodemographic factors
The sociodemographic factors examined in this study were as follows: sex, age, educational level, the status of the basic living recipient, economic activity, and region of residence. Sex was divided into male and female. Age was categorized into three age groups: 65~74 years, 75~84 years, and 85 years or more. Educational level was divided into elementary school or lower and middle school or above by using questions about the educational level and status of graduation. The status of the basic living recipient and economic activity were dichotomously categorized into Yes or No. The region of residence was divided into urban and rural areas.
6) Health-related factors
Regarding the health-related factors of the participants, self-rated health status, smoking, drinking, the frequency of having breakfast during a week, and stress were examined. Self-rated health status was categorized into good (very good or good), fair, and poor (poor or very poor) by using a question about one's usual health status. For smoking, participants were divided into smokers and non-smokers according to the current smoking status. As to drinking, participants were divided into drinkers and non-drinkers by using a question about the experience of drinking alcohol in the past one year. The frequency of having breakfast during a week was divided into 'Having breakfast every day' and 'Not having breakfast every day' by using a question about the frequency of having breakfast during one week in the past one year. Stress was also dichotomously measured by divided the stress level into'Yes (Feel stressed)' or 'No (Not feel stressed)' by using a question about how much the respondent usually feels stressed in daily life.
4. Statistical Analysis
Data analysis was conducted using the SPSS/WIN version 26.0 program. Analysis of complex sample design data was performed by applying the individual weight (wt_p), stratification variable (kstrata), and colony variable (spot_no) presented in the data of the 2020 Korea Community Health Survey to estimate the population. In this study,'Nonresponse', 'Do not know', and 'Not applicable' were treated as missing values, and the rate of missing values of independent variables ranged from 0.01% (smoking) to 13.1% (physical activity). To maintain the sample size and reduce the non-response error, data analysis was conducted by treating missing values as valid values in the complex sample design analysis. The variance inflation factor (VIF) value ranged from 1.01 to 1.93, indicating that there was no multicollinearity among independent variables. The specific analysis methods were as follows.
• Frequencies and percentages were calculated using a complex sample frequency analysis to investigate the rate of depression, factors related to changes in daily life due to COVID-19, factors related to the practice of COVID-19 infection prevention and control rules, factors related to the psychological impact due to COVID-19, sociodemographic factors, and health-related factors among older adults living alone.
• The complex sample Rao-Scott χ2 test was used to investigate differences in depression according to factors related to changes in daily life due to COVID-19, factors related to the practice of COVID-19 infection prevention and control rules, factors related to the psychological impact due to COVID-19, sociodemographic factors, and health-related factors among older adults living alone.
• The complex sample multiple logistic regression analysis was performed by entering independent variables that were found to be significant variables by cross-tabulation analysis to identify factors associated with depression in older adults living alone during the COVID-19 pandemic.
5. Ethical Considerations
The 2020 Korea Community Health Survey was used in this study after obtaining approval from the Statistics Korea (KOSTAT) (Approval No. 117075). The Korea Community Health Survey is de-identified data and does not include personally identifiable information [15], and this study received an exempt determination from the IRB of the relevant institution (IRB No. 4-2021-1402).
|
RESULTS
|
1. The Characteristics and Depression of Older Adults Living Alone
Table 1 shows the results of the complex sample frequency analysis for the characteristics and depression of older adults living alone. Among older adults living alone, the depression group accounted for 6.3%. With respect to factors related to changes in daily life due to COVID-19, 57.8% reported that the level of their physical activity was increased or similar, and 90.4% reported that their sleep hours were increased or similar. The frequency of meeting with friends or neighbors was decreased in 83.5%. Regarding factors related to the practice of COVID-19 infection prevention and control rules, 97.9% performed regular ventilation, but 60.8% did not perform regular disinfection. Most participants reported that they wore a mask indoors or outdoors. 93.8% responded that they kept in touch with close people even though they did not meet together. As for factors related to the psychological impact due to COVID-19, for concerns about COVID-19 infection, the respondents who answered 'Yes' accounted for the largest proportion, and the group who answered 'No' took up the smallest proportion. In the case of concerns about death from COVID-19 infection, concerns about criticism from others due to COVID-19 infection, and concerns about economic damage due to COVID-19, the group who answered'Yes' took up the largest proportion of the responses, and the group who answered 'Average' accounted for the smallest percentage. Regarding the question about the number of people who can help the participant during quarantine treatment or self-quarantine, 74.6% responded that there was at least one person who could help them.
|
With respect to sociodemographic factors, female accounted for 75.7%. As for age, the 65~74 age group made up the largest proportion (47.0%), followed by the 75~84 age group (42.7%) and the age group aged 85 and over (10.3%). As to educational level, people with the educational level of elementary school or lower accounted for 63.9% of the participants. In addition, 81.5% of the participants were not basic living recipients, 75.6% did not do any economic activities, and 67.3% resided in urban areas. In terms of health-related factors, for self-rated health status, 38.4% self-rated their health status as fair, 31.6% as poor, and 30.0% as good. 92.0% were non-smokers, and 72.0% were non-drinkers who did not consume alcohol at all. 88.2% reported that they ate breakfast every day during a week, and 85.4% reported that they did not feel stressed (Table 1).
2. Differences in Depression according to the Characteristics of Older Adults Living Alone
Table 2 shows the results of the complex sample Rao-Scott χ2 test on differences in depression according to the characteristics of older adults living alone. Among older adults living alone, there were significant differences between the depression group and the non-depression group in all variables other than the following variables: wearing a mask outdoors, concerns about COVID-19 infection, concerns about death from COVID-19 infection, concerns about criticism from others due to COVID-19 infection, and sex. The proportions of people reporting decreased physical activity and those reporting decreased sleep hours were higher in the depression group than in the non-depression group. The proportion of people with an increased or similar frequency of meeting with friends or neighbors was also higher in the depression group (p<.001). The depression group showed a lower rate of wearing a mask indoors (p=.004). The rates of performing regular ventilation and regular disinfection were also lower in the depression group, and the rate of not meeting but keeping in touch with close people was also lower in the depression group (p<.001). The depression group showed less concerns about economic damage due to COVID-19, and the proportion of older adults without any persons who can help during quarantine treatment or self-quarantine was higher in the depression group (p<.001).
|
The age of the depression group was higher than that of the non-depression group, and the proportion of people with the educational level of elementary school or lower was higher in the depression group. Also, the proportion of basic living recipients, the proportion of people not doing economic activities, and the proportion of people living in urban areas were higher in the depression group (p<.001). Moreover, the proportion of smokers was higher in the depression group, while the proportion of drinkers was lower in the depression group (p=.003, p=.001). Further, the proportion of people not having breakfast every day during a week was higher in the depression group, and the proportion of people feeling stressed was also higher in the depression group (p<.001) (Table 2).
3. Factors associated with Depression in Older Adults Living Alone during the COVID-19 Pandemic
Table 3 shows the results of the complex sample multiple logistic regression analysis performed to identify factors associated with depression in older adults living alone. The result of calculating the odds ratios for depression in older adults living alone according to independent variables are as follows. First, with respect to the relationship between depression and factors related to changes in daily life due to COVID-19 among older adults living alone, the group of older adults living alone with a decreased amount of physical activity was found to be 1.42 times more likely to have depression than the group with an increased or similar amount of physical activity (95% Confidence Intervals [CI]=1.13~1.78), and the group reporting a decrease in sleep hours was shown to be 2.03 times more likely to have depression than the group with increased or similar sleep hours (95% CI=1.52~2.72). Also, the group with a decreased frequency of meeting with friends or neighbors was 0.69 times less likely to have depression than the group with an increased or similar frequency of meeting with friends or neighbors (95% CI=0.51~0.93). In terms of factors related to the practice of COVID-19 infection prevention and control rules, the group not practicing regular disinfection was 1.31 times more likely to have depression than the group performing regular disinfection (95% CI=1.03~1.67), and the group not wearing a mask indoors was 3.09 times more likely to suffer from depression than the group wearing a mask indoors (95% CI=1.35~7.08).
|
With respect to the association between depression and sociodemographic factors, the ≥85 age group was found to be 1.68 times more likely to have depression than the 65-74 age group (95% CI=1.15~2.46). Also, basic living recipients were 1.57 times more likely to have depression than non-recipients (95% CI=1.22~2.02). Meanwhile, the odds ratio of depression for the group doing economic activities compared to the group not doing economic activities was 0.45 (95% CI=0.33~0.63). In terms of health-related factors, the group with fair self-rated health status and the group with poor self-rated health status were found to be 1.93 times and 6.88 times more likely to have depression, respectively, compared to the group with good self-rated health status (95% CI=1.23~3.03; 95% CI=4.44~10.66). Also, the group not having breakfast every day during a week was shown to be 2.06 times more likely to have depression than the group having breakfast every day (95% CI=1.54~2.75), and the group feeling stressed was found to be 5.42 times more likely to have depression than those not feeling stressed (95% CI=4.35~6.76) (Table 3).
|
DISCUSSION
|
This study attempted to investigate factors associated with depression in older adults living alone during the COVID-19 pandemic. The study results indicated that physical activity, sleep hours, meeting with friends or neighbors, performing regular disinfection, wearing a mask indoors, age, the status of the basic living recipient, economic activity, self-rated health status, the frequency of having breakfast during a week, and stress were associated with depression among older adults living alone during the COVID-19 pandemic.
In this study, the prevalence rate of depression among older adults living alone was 6.3%, which is lower than the prevalence rate of 30.2% in an analysis using the data from the 2017 National Survey of Older Koreans before the outbreak of COVID-19 [19]. In the 2017 National Survey of Older Koreans, depression was assessed using the Short Form of Geriatric Depression Scale (SGDS) [19]. However, it is difficult to make a simple comparison of the prevalence rates of depression because a different depression scale and a different cut-off point were used in this study. On the other hand, the prevalence of depression in this study is higher than the prevalence rate of 5.6% reported in a previous study, which used data from the 2017 Korea Community Health Survey and also used the same scale (the PHQ-9) and the same cut-off point (≥10) as those used in this study [20]. An analysis of data from the 2020 Korea Community Health Survey used in this study showed that the prevalence of depression in older adults with cohabitants during the COVID-19 pandemic was 3.1%, a rate lower than the prevalence of depression in older adults living alone [15]. Although it is difficult to simply compare the prevalence rates of depression due to a lack of studies reporting the accurate prevalence of depression in older adults living alone during the COVID-19 pandemic, a higher prevalence of depression in older adults living alone compared to older adults with cohabitants is consistent with the results of previous studies [12, 13]. However, a study in the U.S. reported that the prevalence of depression in older adults aged 60 years or older during the COVID-19 pandemic was 12.8% [21], which is higher than the result of this study. Therefore, there is a need to repeatedly conduct research on depression in older adults living alone, and it is also required to investigate changes in depression in older adults living alone according to the degree of the spread of the COVID-19 pandemic and the periods during the COVID-19 pandemic.
In this study, the rate of depression was higher in the group with decreased physical activity than in the group with an increased or similar amount of physical activity among older adults living alone. This result is in agreement with the previous research finding that decreased walking was related to a higher rate of depression in older adults aged 65 or older during the COVID-19 pandemic [6]. As older adults are forced to stay at home due to restrictions on participation in social activity during the COVID-19 pandemic, it is necessary to prevent their depression through regular physical activity to ensure that older adults living alone can maintain healthy and independent life. In this connection, a previous study reported that home-based exercise was found to be effective in stopping the reduction of physical activity and sedentary lifestyle in older adults during the COVID-19 pandemic [22]. Based on these research results, it is considered necessary to provide home-based physical activity nursing intervention programs, and develop community health policies related to such interventions.
In this study, the rate of depression was higher in the group with decreased sleep hours than in the group with increased or similar sleep hours among older adults living alone. In relation to the relationship between depression and sleep duration, previous studies reported diverse research results. Mishra et al. [23] found that a greater decrease in sleep duration was associated with a higher level of depression in older adults during the COVID-19 pandemic. However, a study of the relationship between daily behaviors, depression, and anxiety in older adults during the COVID-19 pandemic found that the level of depression was higher in the groups with increased or decreased sleep duration than in the group without any changes in sleep duration [6]. However, a reduction in sleep duration is known to cause changes in cortisol, a steroid hormone, and thereby increase depression [24], and changes in sleep duration have been reported to affect mental health in older adults during the COVID-19 pandemic [6, 23]. Therefore, it is necessary to conduct a longitudinal study of older adults to elucidate the causal relationship between sleep and depression in older adults and examine the cause of the decrease of sleep duration in older adults.
In this study, the rate of depression was lower in the group with a decreased frequency of meeting with friends or neighbors than in the group with an increased or similar frequency of meeting with friends or neighbors. This result is in contrast with the finding in a previous study that face-to-face social networks decreased the rate of depression in older adults after the outbreak of the COVID-19 pandemic [25]. Meanwhile, a previous study examined the status of living alone, social contact and emotional health in older adults during the COVID-19 pandemic, and reported that older adults living alone showed a greater response to social contact and they tended to meet friends more frequently than family members [26]. The results of this study seem to show that non-face-to-face social interactions such as phone calls played the role of alleviating depression in older adults living alone during the COVID-19 pandemic [27]. In view of these study results, there is a need to provide programs to form and support social networks including non-face-to-face social networks in order to prevent depression in older adults living alone.
Among factors related to the practice of COVID-19 infection prevention and control rules, the rate of depression was higher in the group not performing regular disinfection and in the group not wearing a mask indoors. This result is consistent with the previous finding that preventive behaviors against COVID-19 were associated with the decrease of depression in older adults [9]. In a study of the use of masks of older adults living alone during the COVID-19 pandemic, it was found that the majority of older adults living alone wore masks when going out, but most of them were not able to purchase them for themselves [28]. This is presumed to be due to the fact that older adults living alone may have difficulty in purchasing masks due to financial problems considering that the proportion of basic living recipients is higher in older adults living alone than in older adults with cohabitants, and many of them do not perform economic activities. Therefore, it is necessary to provide older adults living alone with items needed for practicing COVID-19-related infection prevention and control in daily life, and provide tailored educational programs on the practice of personal rules for infection prevention in order to encourage older adults living alone to properly practice personal rules for infection prevention and control in daily life.
In this study, among older adults living alone, the ≥85 age group showed a higher rate of depression than the 65~74 age group. This result is similar to the finding in a previous study that the rate of depression increased with the increase of age [14]. However, this result is not consistent with a previous study which compared risk factors for depression between older adults living alone and older adults with cohabitants, and reported that age was not related to depression in older adults living alone [13]. In addition, this study found that among older adults living alone, basic living recipients and older adults not doing economic activities showed a higher rate of depression. These results are in agreement with the finding in a previous study that the rate of depression was higher in basic living recipients among older adults living alone [13]. The results are also similar to the finding of a previous study that lower socioeconomic status was associated with a higher rate of depression [14]. These results are thought to indicate that economically vulnerable older adults showed an increased rate of depression because they could experience real limitations such as restrictions on daily life and reduced social contact [29]. Therefore, to prevent depression in older adults living alone, it is necessary to provide depression prevention interventions for economically vulnerable older adults living alone.
In older adults living alone, poorer self-rated health status was related to a higher rate of depression, and this result is consistent with a previous study [14]. In addition, among older adults living alone, the rate of depression was higher in the group not having breakfast every day during a week than the group having breakfast every day. This result is similar to the finding in a previous study that the rate of depression was lower in older adults regularly having six meals during the past two days [30]. Furthermore, this study found that the rate of depression was higher in the group feeling stressed among older adults living alone, and this finding is consistent with the result of a previous study that stress was associated with a higher level of depression [12]. This study finding is thought to reflect the situation in which social isolation and loneliness due to the decrease of participation in social activities during the COVID-19 pandemic may lead to a deterioration of health status and also act as a cause of stress in older adults living alone, thereby increasing the level of depression in them.
The following limitations of this study should be mentioned. First, this study is a secondary data analysis study using the data from the 2020 Korea Community Health Survey, and thus it was not possible to include variables related to chronic diseases in the analysis. In other words, since the data of the 2020 Korea Community Health Survey included only items on hypertension and diabetes mellitus regarding chronic diseases, it was difficult to include various kinds of chronic diseases in the analysis. Second, in this study, in the depression group of older adults living alone, the total number of people not wearing a mask indoors was 15, a relatively smaller figure than the number of people wearing a mask indoors. Since this fact may have affected sampling error, some caution is required in interpreting the study results. Third, since this study was conducted only with some older adults living alone, there is a limitation in generalizing and applying the results of this study to all older adults living alone. However, this study attempted to overcome this problem by conducting a complex sample design analysis to estimate the population.
|
CONCLUSION
|
This study examined the prevalence rate of depression in older adults living alone during the COVID-19 pandemic, and identified factors associated with depression in older adults living alone during the COVID-19 pandemic by using a large-scale data representative of the national population of Korea. In this study, physical activity, sleep hours, meeting with friends or neighbors, performing regular disinfection, wearing a mask indoors, age, the status of the basic living recipient, economic activity, self-rated health status, the frequency of having breakfast during a week, and stress were found to be associated with depression in older adults living alone during the COVID-19 pandemic. The results of this study suggest that there is a need to develop tailored interventions to prevent and manage depression in older adults living alone by taking into account factors associated with depression in older adults living alone during the COVID-19 pandemic.
|
Notes
|
Research Grant: This research was supported by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education (No. NRF-2020R1A6A1A03041989).
|
References
|

 KACHN
KACHN




 Cite
Cite

