Articles
- Page Path
- HOME > J Korean Acad Community Health Nurs > Volume 33(4); 2022 > Article
- Original Article Educational Status and Needs of Premature Birth Prevention and Its Association with Preconception Health Behavior among Women of Childbearing Age in Korea
- Sun Hee Kim1, Ji-Yeon Hong2*, Mi Kyung Park2
-
DOI: https://doi.org/10.12799/jkachn.2022.33.4.372
Published online: December 31, 2022

2Graduate School Student, College of Nursing, Daegu Catholic University, Daegu, Korea

-
*Corresponding email:
solid1212@naver.com
- 925 Views
- 43 Download
- 2 Crossref
- 0 Scopus
Abstract
Purpose
The aim of this study was to investigate the educational status and needs of premature birth prevention, and to identify factors associated with preconception health behaviors.
Methods: The study design was a crosssectional descriptive study. Data were collected through an online questionnaire survey, and the subjects were 192 women of childbearing age in Korea. Data were analyzed using the Mann-Whitney U test, Kruskal-Wallis test, Spearman's correlation coefficients, and multiple regression.
Results: The proportion of subjects who received education on premature birth prevention was 8.9%, and 75.5% of subjects answered that they needed education on premature birth prevention. They demanded education through online media, small groups, cases, cartoons (webtoon) with stories, pictures, and videos. A related factor of preconception health behavior was self-efficacy for high-risk pregnancy health care (β=.20, p=.012), which accounted for 8.2% of the total variance related to preconception health behavior.
Conclusion: There was a need for more development of education programs to prevent premature birth for women of childbearing age. Its education programs should be applied with online, small group activities using various educational media. It is also required to promote preconception health behavior through self-efficacy for high-risk pregnancy health care.
| J Korean Acad Community Health Nurs. 2022 Dec;33(4):372-384. English. Published online Dec 30, 2022. https://doi.org/10.12799/jkachn.2022.33.4.372 | |
| © 2022 Korean Academy of Community Health Nursing | |
Sun-Hee Kim ,1
Ji-Yeon Hong ,1
Ji-Yeon Hong ,2
and Mi Kyung Park ,2
and Mi Kyung Park 2 2
| |
|
1Professor, College of Nursing, Research Institute of Nursing Science, Daegu Catholic University, Daegu, Korea. | |
|
2Graduate School Student, College of Nursing, Daegu Catholic University, Daegu, Korea. | |
Corresponding author: Hong, Ji-Yeon. College of Nursing, Daegu Catholic University, 33 Duryugongwon-ro, 17-gil, Nam-gu, Daegu 42472, Korea. Tel: +82-53-650-4831, Fax: +82-53-650-4392, | |
| Received July 08, 2022; Revised September 13, 2022; Accepted September 27, 2022. | |
|
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by- | |
|
Abstract
| |
|
Purpose
The aim of this study was to investigate the educational status and needs of premature birth prevention, and to identify factors associated with preconception health behaviors.
Methods
The study design was a cross-sectional descriptive study. Data were collected through an online questionnaire survey, and the subjects were 192 women of childbearing age in Korea. Data were analyzed using the Mann-Whitney U test, Kruskal-Wallis test, Spearman's correlation coefficients, and multiple regression.
Results
The proportion of subjects who received education on premature birth prevention was 8.9%, and 75.5% of subjects answered that they needed education on premature birth prevention. They demanded education through online media, small groups, cases, cartoons (webtoon) with stories, pictures, and videos. A related factor of preconception health behavior was self-efficacy for high-risk pregnancy health care (β=.20, p=.012), which accounted for 8.2% of the total variance related to preconception health behavior.
Conclusion
There was a need for more development of education programs to prevent premature birth for women of childbearing age. Its education programs should be applied with online, small group activities using various educational media. It is also required to promote preconception health behavior through self-efficacy for high-risk pregnancy health care. |
|
Keywords:
Educational status; Health behavior; Needs assessment; Preconception care; Premature birth
|
|
|
INTRODUCTION
|
Premature birth is defined as the birth of babies before 37 weeks of pregnancy have been completed, it is a major cause of death in children under five years of age, and it is a worldwide problem since it accounts for an average of 5~18% of live births in countries around the world [1]. The premature birth rate in Korea has continued to increase from 5.8% in 2010 to 8.5% in 2020 [2], and the primary cause is that the fertility rate of women aged 35 and older has increased from 18% in 2011 to 33.8% in 2020 [2, 3].
The causes and risk factors of premature birth include a history of obstetrical and gynecological disorders such as a previous history of preterm delivery, cervical surgery, and genital infection, demographic factors such as maternal age, race, and low socioeconomic status, nutritional and physical activity factors such as body weight and dietary intake, health behavior factors such as smoking, drinking, drug abuse, and exercise, psychological factors such as depression and stress, pregnancy-related factors such as birth interval, infertility treatment, premature rupture of membranes, preterm labor, placenta praevia, placental abruption, polyhydramnios, and oligohydramnios, and environmental factors such as radiation and fine dust [4, 5]. In addition, all preconception women and pregnant women may have biological, psychological, social and clinical risk factors for premature birth, depending on how they manage their health [6]. Among these risk factors, controllable risk factors, including women's demographic factors, nutritional and physical activity factors, health behavior factors, psychological factors, and pregnancy-related factors, allow us to reduce the risk of premature birth through preventive management and active response strategies.
Meanwhile, high-risk pregnancy is generally defined as the state of pregnancy that involves higher risk for the illness or death of the pregnant woman, the fetus or both than in cases of normal pregnancy, and has risk factors for high-risk pregnancy that may affect pregnancy outcomes [7]. The most common risk factor for high-risk pregnancy is maternal age, and other representative risk factors are as follows: 1) preconception health status such as obesity, hypertension, diabetes, and autoimmune diseases; 2) previous pregnancy history such as cervical incompetence, preterm labor, preeclampsia, and gestational diabetes mellitus (GDM); 3) diseases occurring during pregnancy such as excessive or poor maternal weight gain during pregnancy, preeclampsia, GDM, preterm labor, multiple pregnancy, hemorrhagic placental disorders, amniotic fluid disorders, cervical incompetence, and chorioamnionitis; and 4) fetus problems such as fetal malformations and intrauterine growth retardation [7]. These demographic characteristics and risk factors for high-risk preconception and pregnancy eventually become risk factors for premature birth, and high-risk pregnancy can be seen as pregnancy involving risk factors for premature birth. Therefore, considering that high-risk pregnancy is closely linked to premature birth, high-risk pregnancy health care can be regarded as activities for premature birth prevention (PBP). Although health behaviors during pregnancy are also important for PBP, premature birth can be prevented through preconception health behaviors (PHBs) to control risk factors for high-risk pregnancy [4, 5]. For this reason, it is important to understand how PHBs influence future pregnancy and to manage potential risk factors [8].
The preconception period is an important period for the PBP, and PHBs can lead to better pregnancy outcomes by changing women's risk behaviors [6]. In other words, premature birth can be prevented through health behaviors to manage factors such as chronic diseases, anemia, sexually transmitted infections, smoking, mental health problems, birth spacing, vaccination to prevent fetal malformations, folic acid and adequate nutrient intake, and obesity [9, 10]. However, Korea's policies related to pregnancy and childbirth are mainly centered on the increase of the number of live births in relation to the low birth rate, and since government policies are focused on postnatal care approaches, there is still a lack of preventive approaches related to preconception health care [11]. In addition, although many women have a positive attitude toward preconception care, they often do not consider it necessary for themselves [12]. Thus, since the investigation of influencing factors for PHBs among women of childbearing age (WCA) can be viewed as the exploration of factors associated with activities for PBP, the identification of factors affecting PHBs is required for the development of interventions for PBP.
The promotion of knowledge of PBP helps WCA to become aware of and perform health behaviors for PBP [13], According to the self-management theory, individuals can practice health behaviors if they have knowledge about behaviors, self-regulation skills and ability to modify health behaviors, and social support [14]. Especially, self-efficacy is an important factor for health care since it enables individuals to select active response strategies, overcome obstacles, and eventually solve problems in an efficient manner [15], In pregnant women at risk of premature birth, a higher level of self-efficacy has been reported to be associated with better practice of health behaviors [16], so WCA with a high level of knowledge of high-risk pregnancy health care (K-HRPHC) and a high level of self-efficacy for high-risk pregnancy health care (SE-HRPHC) are expected to properly practice PHBs. However, there has been a lack of studies that have elucidated the relationship of PHB with K-HRPHC and with SE-HRPHC.
According to previous studies, WCA in Korea showed a moderate level of PHBs [17], and they were also found to have a moderate level of K-HRPHC and a moderate level of SE-HRPHC in [18]. In addition, preconception education has been shown to influence changes in knowledge about nutrition, lifestyle, and physical health [19]. It has also been reported that since the promotion of knowledge about the PBP increases health behaviors for the PBP, new prevention programs reflecting the methods of communication and needs of WCA need to be developed in order to enhance knowledge of PBP [13]. Thus, to identify the commonly used methods of communication and needs of WCA, it is necessary to investigate the current status of education on PBP for WCA as well as effective and preferred methods of education among WCA.
Since WCA are persons that may be at risk of premature birth and need to practice preventive behaviors before pregnancy or during early pregnancy, it is most important for these women to be aware of and practice health behaviors for PBP. However, intervention programs for PBP reported so far have been focused on examining the symptoms of preterm labor and ensuring that the patient will receive appropriate medical treatment [13]. In other words, although regular prenatal care and the operation of multidisciplinary PBP clinics composed of maternal-fetal medicine specialists, nurses, nutritionists, and social workers have been attempted as new preventive approaches, the main prevention program consisted of more frequent prenatal hospital visits and patient education on the signs and symptoms of premature birth, and this method did not lead to a decrease in the premature birth rate [13]. On the other hand, smoking cessation using counseling and peer support for pregnant women in early pregnancy and the smoke-free law [20] and prenatal nutrition education on increasing energy and protein intake for general pregnant women [21] were reported to be effective in reducing the premature birth rate. In other words, PBP programs reported so far have been education on hospital-centered prevention focused on medical examination and symptom recognition using prenatal hospital visits along with early hospital visits, and only programs for intensive management of specific health behaviors such as smoking cessation and nutrition during pregnancy have been reported.
The PBP requires long-term, diverse, and combined health care activities, so the first task for the development of programs for the comprehensive management of such health care activities to prevent premature birth is to identify the educational status and needs of PBP implemented in Korea. In addition, since K-HRPHC, SE-HRPHC, and PHBs of WCA are capabilities required for the PBP, there is a need to investigate the status of these factors. Thus, this study aimed to investigate the educational status and needs of the PBP by examining the experience of education on the PBP, K-HRPHC, SE-HRPHC, and PHBs among WCA. The specific objectives of this study are as follows:
• To examine the contents, methods, and types of information and communications technology (ICT) of education on the PBP experienced by WCA;
• To examine the contents, methods, and types of ICT of education on the PBP needed by WCA;
• To investigate correlations between K-HRPHC, SE-HRPHC, and PHB among WCA;
• To identify factors affecting PHBs among WCA.
|
METHODS
|
1. Study Design
This study is a cross-sectional descriptive study to investigate the educational status and needs of the PBP and identify factors affecting PHBs in WCA.
2. Participants
The participants were WCA residing in Korea. The specific inclusion criteria were WCA in the 20~49 age group residing in Korea, persons who can read and write text content on mobile devices or computers, and persons who understood the purpose of this study and voluntarily signed the informed consent form. The sample size was calculated using the G*Power 3.1.9.2 program, and when it was calculated using a medium effect size of 0.5, the level of significance of .05, power of .80, 12 predictor variables, and a two-tail test in a multiple regression analysis, the minimum number of participants needed for this study was determined to be 127 persons. Therefore, the questionnaire survey data was collected from 200 participants in consideration of the drop-out rate of 30% of an online questionnaire survey, and the data of 192 persons (96%) were used for the final analysis, excluding eight questionnaires with missing or insufficient responses.
3. Measures
1) Educational status and needs of the PBP
To investigate the status of education on the PBP, it was first examined whether each subject had the experience of receiving education on the PBP, and the subjects without any experience of education were asked about the reason for not receiving the education. Also, the contents, methods, and types of ICT of the education they received, the level of knowledge of PBP, and the level of satisfaction with education on the PBP were examined among the participants with the experience of education on PBP. Among the survey items, the contents of education were divided into the contents of primary, secondary, and tertiary prevention. Regarding the contents of education, primary prevention was about the prevention and delay of premature birth before the occurrence of premature birth, and secondary prevention was about early detection and treatment of the symptoms of premature birth. The contents of tertiary prevention included the prevention of aggravation and disabilities and rehabilitation after pregnant women are in a dangerous situation of having a premature birth. Additionally, the level of satisfaction with education on the PBP was examined regarding the method of education and type of ICT.
To investigate the needs for education on the PBP, educational contents, the method of education, the type of ICT, and needs for education were examined among all the participants.
2) K-HRPHC
The tool used to assess K-HRPHC was the pregnancy health care knowledge scale for pregnant women of advanced maternal age developed by Wang and Kim [16]. To use this scale in this study, it was slightly modified by the researcher. Only one item of the original version was modified by changing 'the possibility of caesarean section' to 'the possibility of premature birth.' This instrument is composed of a total of 10 items: 1 item on risk factors for premature birth, 3 items on the management of dangerous symptoms during pregnancy, 5 items on the management of health problems during pregnancy, and 1 item on exercise management during pregnancy. The items included statements such as 'It is normal for your face to swell in the evening during pregnancy', 'If you notice a few small spots of blood on your underwear without abdominal pain, you should take a rest at home', and 'If you work standing for a long time, you may have a premature birth.' 1 point was given for each correct answer, and the total scores ranged from 0 to 10 points. Higher scores indicate higher levels of K-HRPHC. The content validity index (CVI) of the original version of this scale was reported to be .88 [16], and Cronbach's α was .70 in this study.
3) SE-HRPHC
The SE-HRPHC was measured using the pregnancy care self-efficacy scale for pregnant women of advanced maternal age developed by Wang & Kim [16]. This instrument was slightly modified and used in this study, and only one item of the original version was modified by changing'advanced-age pregnancy' into 'age.' This self-efficacy assessment tool consists of a total of 16 items: 2 items on the understanding of pregnancy, 4 items on the management of risk symptoms during pregnancy, 3 items on the management of health problems during pregnancy, 4 items on the management of nutrition during pregnancy, 2 items on the management of daily living activities, and 1 item on emotion management during pregnancy. The survey items include statements such as 'I can describe the effects of maternal age on pregnancy', 'If I have vaginal bleeding, I can appropriately deal with this problem', and 'I know the symptoms of pregnancy-induced hypertension (PIH) and can appropriately deal with (manage) this disease.' Each item was measured on a 5-point Likert scale ranging from 1 point='Strongly agree' to 5 points='Strongly disagree.'The total scores ranged from 16 to 80 points, and higher scores indicated higher levels of SE-HRPHC. Regarding the reliability of the total items, Cronbach's α of the original instrument was .89 [16], and Cronbach's α was .88 in this study.
4) PHB
PHB was assessed by the instrument developed by Yeom & Kim [15]. This tool consists of 6 domains and 27 items. More specifically, it is comprised of 4 items on the avoidance of hazardous materials, 6 items on professional health care, 4 items on rest and sleep, 4 items on stress management, 5 items on information acquisition, and 4 items on the preparation of resources. The items included statements such as 'I do not smoke or drink', 'If you are 35 years old or older, you should consult healthcare professionals about genetic risks and necessity for prenatal care', and 'I do not lift or carry heavy objects.' Each item was measured on a 5-point Likert scale ranging from 1 point='Very unlikely' from 5 points='Very likely.' The total scores ranged from 27 to 135 points, and higher scores indicate higher levels of PHBs. Cronbach's α of the total items of the original instrument was .92 [15], and Cronbach's α was .95 in this study.
5) General and obstetrical characteristics of participants
As to the general characteristics of participants, age, education level, occupation, marital status, family monthly income, and region of residence were examined. In addition, regarding obstetrical characteristics, the experience of childbirth, the number of children, premature birth history, cause of premature birth, disease related to pregnancy or childbirth, intention to give birth, and the self-perceived possibility of premature birth were examined.
4. Ethical Considerations
This study was conducted after obtaining approval from the IRB of Daegu Catholic University (CUIRB-2021-0043). The participants were provided with explanations about the purpose and contents of this study, anonymity and confidentiality of the collected data, and no disadvantages due to participation in this study. In addition, the participants were provided with a participant information sheet stating that the collected data will be used only for the purpose of research and they are allowed to withdraw from the study at any time if they want to. They were requested to respond to the online questionnaire only after they read and fully understood the contents of the participant information sheet and provided written informed consent.
5. Data Collection
The data was collected from August 24, 2021 to September 2, 2021. Regarding the data collection method, research assistants residing in seven large cities (7 Metropolitan Cities) and 5 provinces in South Korea posted a promotional announcement about the questionnaire survey on their SNS pages. The survey announcement included the purpose of the study, inclusion criteria, method and period of participation, benefits for participants, and confidentiality and anonymity of the collected data. It also included a link to the survey, and persons who voluntarily wanted to participate were asked to participate in the survey by clicking on a URL link included in the promotional document. Each participant who completed the online questionnaire was given a coffee coupon as a small token of appreciation.
6. Statistical Analysis
The analysis of the collected data was conducted using IBM SPSS statistics for Window Version 25.0 (IBM Co., Armonk, NY, USA). The normality test was carried out using the Kolmogorov-Smirnov test, and a non-parametric test was used for variables that did not meet the normality assumption. The general characteristics, characteristics related to pregnancy and childbirth, and the educational status and needs of PBP of the participants were analyzed using descriptive statistics such as the frequency, percentage, mean, and standard deviation. Also, the Mann-Whitney U test and Kruskal-Wallis test were used to analyze differences in PHB according to general characteristics, characteristics related to pregnancy and childbirth, and the educational status and needs of PBP of the participants. In addition, posthoc tests were performed using the Mann-Whitney U test. Correlations between K-HRPHC, SE-HRPHC, and PHBs were analyzed using Spearman's correlation coefficients (rho, ρ). Multiple regression analysis (simultaneous entry method) was conducted to identify factors affecting PHB.
|
RESULTS
|
1. General and Obstetrical Characteristics of Participants
The mean age of the participants was 32.70±7.20 years, and 85 persons (44.3%) belonged to the 30~39 age group, constituting the largest proportion of the total participants. As for educational level, college graduates were 141 persons (73.4%), and people with occupations were 129 persons (67.2%), accounting for the largest proportion. As to marital status, married people were 110 persons (57.3%), and regarding family monthly income, 50 persons (26.0%) had a family monthly income of 7 million or more, accounting for the largest proportion. For the residential area, 93 persons (48.4%) lived in a metropolis.
In terms of obstetrical characteristics, 92 persons (47.9%) had childbirth experience, and 49 persons (53.3%) had two or more children. Among them, 11 persons (12%) experienced premature birth and 8 person (72.7%) experienced premature birth due to maternal causes. In addition, 18 participants (9.4%) reported having diseases related to pregnancy or childbirth. Regarding the health problems the participants were diagnosed with, the results of a multiple-response survey showed that GDM (6 persons) accounted for the highest proportion, followed by abortion (5 persons), PIH (2 persons), premature birth (2 persons), and benign uterine or ovarian tumor (2 persons). 71 persons (37.0%) responded that they had the intention to give birth in the future. As to the self-perceived possibility of premature birth, 44 persons (23.0%) answered that there is a 'high possibility' (Table 1).
|
2. Educational Status and Needs of the PBP
The analysis results of the educational status and needs of the PBP are shown in Table 2. First, regarding the status of education on the PBP, it was found that 17 persons (8.9%) had experience receiving education on PBP, while 175 persons (91.1%) did not have any experience. As to the reasons for not receiving education on PBP, one participant did not respond, and among the 174 persons who gave responses, 71 persons (40.8%) answered that there was no information or education available, 42 persons (24.1%) responded that they did not have a chance or time for it, 40 persons (23.0%) stated that they did not know what education or information was required for them, and 21 persons (12.1%) did not feel the need for education. The contents of education experienced by 17 participants with experience in education on PBP were examined using a multiple-response question. As a result, the most frequently experienced contents of education were as follows:'risk factors and causes of premature birth' (16 persons) and 'the baby's viability and health problems by the week of gestation' (16 persons) for the first prevention education;'prenatal hospital visits and treatment of women at high risk of premature birth' (14 persons) and 'premature birth or risk symptoms of the mother and fetus' for the secondary prevention education (14 persons); and 'longterm health problems of a baby after premature birth' (11 persons) for the tertiary prevention education (Appendix 1). Regarding the methods of education, the most frequently used methods were 'booklet or pamphlet' (11 persons) and 'information in the form of text' (16 persons). Regarding the satisfactory methods of education, the largest proportion of the respondents selected 'large group traditional (face-to-face) setting' (4 persons) and 'small group traditional (face-to-face) setting' (4 persons). The most satisfactory types of ICT were identified as videos (5 persons) and cases (5 persons). As for the self-perceived level of knowledge of PBP, out of the total participants, 8 persons (4.1%) gave the response 'Knew well', 51 persons (26.6%) rated their level of knowledge as 'Moderate', and 133 persons (69.3%) gave the response 'Not know well.'
|
With respect to the needs for PBP education among all the participants, the scores of needs for education were 4.52±0.52 points for primary education, 4.56±0.53 points for secondary education, and 4.47±0.61 points for tertiary education, showing the overall strong needs for all of the first, secondary and tertiary prevention education. As to the method of PBP education, 'YouTube' was the most preferred method of education (72 persons, 37.5%), followed by a 'small group traditional (face-to-face) setting' (39 persons, 20.3%). As for the type of ICT of education, the participants showed the strongest need for 'cases' (4.50±0.68 points), followed by 'webtoons (cartoons) with stories' (4.10±0.94 points), and 'pictures' (4.07±0.84 points). Regarding the necessity for education for PBP, the largest proportion of the respondents (145 persons, 75.5%) answered'Necessary,'
3. K-HRPHC, SE-HRPHC, and PHB
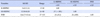
The mean score for K-HRPHC was 5.42±2.11 points, the mean score for SE-HRPHC was 52.30±8.83 points (the mean item score: 3.27 points), and the mean score for PHB was 114.17±15.64 points (the mean item score: 4.23 points) (Table 3).
|
4. Differences in PHBs
The examination of differences in PHBs according to the characteristics of participants showed that there were no significant differences in PHBs depending on the general or obstetrical characteristics of the participants. In relation to the educational status and needs of the PBP, there was a significant difference in PHB depending on the level of knowledge of PBP (χ2=5.99, p=.049), and the results of post-hoc analysis showed that the level of PHB was higher in the group that gave the response 'Knew well' in response to the question about knowledge of PBP than in the group that replied as 'Did not know well' (Table 4).
|
5. Correlations between K-HRPHC, SE-HRPHC, and PHB
K-HRPHC was found to have a significant positive correlation with SE-HRPHC (ρ=.37, p<.001) and with PHBs (ρ=.18, p=.012). In addition, SE-HRPHC was also shown to have a significant positive correlation with PHB (ρ=.21, p=.003) (Table 3).
6. Factors associated with PHBs
To examine factors associated with PHB, analysis was performed by entering K-HRPHC, SE-HRPHC, and knowledge of PBP as independent variables. Knowledge of PBP measured by a nominal scale was entered as an independent variable after converting it into a dummy variable. Tests for autocorrelation of the dependent variable and multicollinearity between independent variables were performed. The Durbin-Watson index was 1.95, a value close to 2, indicating that there was no autocorrelation of error terms. The variance inflation factor (VIF) ranged from 1.10 to 1.25, indicating that there was no multicollinearity between independent variables.
SE-HRPHC was identified as a factor associated with PHB (β=.20, p=.012), the explanatory power of this model was 8.2%, and the regression model was statistically significant (F=4.20, p=.003) (Table 5).
|
|
DISCUSSION
|
This study attempted to investigate the educational status and needs of the PBP among WCA residing in Korea, measure PHB to examine preconception behavior for PBP, and identify factors associated with PHB. The analysis results of this study revealed a low percentage of recipients of education on PBP and the preferred methods of education as well as methods of education with a high level of satisfaction among WCA. In addition, SE-HRPHC was identified as a factor associated with PHB for the PBP.
In particular, the investigation of the status of education on the PBP showed that the proportion of the participants with health problems related to pregnancy and childbirth, which constitute risk factors for premature birth, was less than 10% (specifically, 9.4%). Their health problems related to pregnancy and childbirth included GDM, abortion, premature labor, and benign uterine or ovarian tumor. These health problems during pregnancy are similar to the results of a previous study on the status of prenatal health management in Korean pregnant women [22], which reported that the main health problems of Korean pregnant women were found to be GDM, premature labor, gestational hypertension, and cervical incompetence. Therefore, to obtain maximum effects with minimum management for the high-risk group for premature birth that accounts for less than 10% of WCA, a stepwise, preventive approach is required. In other words, to prevent premature birth due to high-risk pregnancy, it is necessary to manage controllable factors from the preconception period, predict and selectively identify risk factors for high-risk pregnancy, and thereby establish a stepwise long-term health management system for early management for women with a high possibility of high-risk pregnancy or at an early stage of detection of high-risk pregnancy.
In this study, the participants were found to have high needs for education on PBP regarding the overall prevention interventions from the primary prevention to the tertiary prevention. However, the majority of the participants of this study did not have the experience of receiving education on PBP, and the participants reported that the reasons for not receiving education were the absence of information and educational programs available, a lack of time, and the lack of knowledge about information and education needed for them. The absence of specialized information and education is thought to indicate a limitation of publicity and accessibility of public health promotion, and the lack of time and the lack of knowledge about information and education needed are considered to be due to a lack of recognition of negative consequences of premature birth and the necessity for management. In this regard, it has been reported that most women have not heard of the term premature birth before or do not know well about premature birth [23], and most women without the experience of high-risk pregnancy did not know their risk factors until they went to the hospital and consulted a healthcare professional about their health risks [24]. The recognition of the risk of premature birth is likely to induce prevention behaviors and early interventions, and thus lead to healthy pregnancy outcomes [25], so there is a need for information and educational interventions on premature birth.
With respect to the method of education on the PBP, the most common method of education among the participants was 'booklets or pamphlets,' and the participants showed a low level of satisfaction with this method. In this study, the method of education most preferred by the participants was YouTube, followed by small group offline (face-to-face) educational programs, websites operated by a hospital or an expert, SNS (Instagram, Facebook, etc.), and mobile applications in descending order. These results indicated that WCA have a greater need for easily accessible and easy-to-use online media than other methods of education, and prefer 'small group' education to 'large group' education. These results are in agreement with the findings of a previous study showing that 56.6% of pregnant women wanted to receive prenatal education through online programs [18] and another previous study reporting that an online method was found to be the most preferred path for obtaining information on preconception health [25]. Furthermore, in previous studies, the effectiveness of mobile web-based educational programs [18] and the positive effects of preconception health care through websites [26] were confirmed. These findings also show the need for developing educational programs using online media.
In this study, the most common type of ICT used in the education on PBP was 'information in the form of text', and the level of satisfaction with this type of ICT was also found to be low. In terms of the type of ICT, the participants showed the highest level of satisfaction with videos and cases, and had the greatest demand for cases, followed by webtoons (cartoons) with stories, pictures, and videos. A previous study also reported that educational materials in the form of videos were found to be more effective in the improvement of genetic knowledge than those in the form of text [27]. Therefore, the results of this study along with the findings of previous studies are thought to indicate that cases with stories facilitate a concrete understanding and application of educational contents, and WCA prefer educational materials that present information in easily comprehensible pictures or videos.
Preconception health status such as underlying diseases, obesity, infections, smoking, and drug addiction, and health behaviors to remedy such health problems have been shown to be important determinants for childbirth outcomes such as premature birth [6]. Thus, this study investigated factors related to PHBs for the PBP among WCA, and as a result, SE-HRPHC was found to be a single factor increasing PHBs. In this connection, according to previous studies, preconception health education can improve self-efficacy for health [28], self-efficacy was found to be a factor directly related to healthy eating habits [29], and observational learning for the promotion of self-efficacy was found to be the most important determinant for the increase of physical activity [30]. Therefore, if SE-HRPHC is improved through educational interventions for PBP, it is expected to contribute to increasing PHBs through healthy eating habits and physical activity. In addition, this study attempted to identify factors related to PHBs that can be viewed as PBP behaviors by exploring demographic and obstetrical characteristics, the status and needs of education for PBP, K-HRPHC, and SE-HRPHC among WCA before pregnancy rather than during pregnancy. As a result, only SE-HRPHC was found to be significantly associated with PHBs, and this factor explained only 8.2% of the total variance. This may be due to the fact that although the participants recognized the importance of PHBs, they did not consider it necessary for themselves to practice PHBs [12]. On the other hand, in this study, the mean score for PHBs was 114.17 points (the mean item score: 4.23 out of 5 points), showing upward bias, so there is a possibility that the practice of PHBs was not properly evaluated because the participants did not actually have a plan or intention to give birth in the very near future at the time of their participation in the survey. Therefore, in future studies, it is necessary to conduct research with women with an intention to give birth in the immediate or very near future and perform analyses by adding variables not dealt with in this study, such as the prenatal care system of public medical institutions.
This study investigated the status and needs of education for PBP among WCA that have not been sufficiently studied in Korea as well as in other countries, and also examined the participants' levels of K-HRPHC and SE-HRPHC, which are variables not analyzed in previous studies. As a result, this study presented directions for the development of PHB interventions for the PBP. In addition, this study was carried out with WCA selected by convenience sampling among those residing in seven Metropolitan Cities, and 5 provinces in Korea. However, since there were only a small number of participants with experience in education on the PBP, this study has the following limitations. First, there is a limitation in generalizing the study results on the educational status and needs of the PBP. Second, it was not possible to conduct a thorough and in-depth analysis of the specific status and needs of education for PBP.
|
CONCLUSION
|
The participants of this study mostly received primary PBP education among primary, secondary, and tertiary prevention education, and the percentage of the recipients of education for PBP was less than 10%. These results showed the necessity for the development of step-wise and long-term educational interventions for the PBP. In addition, WCA showed greater needs for Internet-based information, small-group education, and educational materials with cases, pictures, and videos. Further, it was found that it is necessary to apply programs for the improvement of SE-HRPHC in order to enhance PHBs for the PBP.
In this study, analysis results revealed a low explanatory power of the factor associated with PHBs, so there is a need to conduct a replication study by including diverse factors affecting PHBs. In addition, it is suggested to conduct further research among WCA with the experience of PBP education in order to carry out an in-depth investigation of educational interventions for the PBP in the future.
|
Notes
|
This research was supported by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education (2021R1I1A3047489)
|
References
|

 KACHN
KACHN





 Cite
Cite

