Articles
- Page Path
- HOME > Res Community Public Health Nurs > Volume 34(4); 2023 > Article
-
Original Article
- Development and Effectiveness of a Basic Epidemiological Investigation Simulation Program of Emerging Respiratory Infectious Diseases for Nursing Students: Application of Standardized Patients
-
Jiyun Park1
 , Gye Jeong Yeom2
, Gye Jeong Yeom2
-
Research in Community and Public Health Nursing 2023;34(4):267-280.
DOI: https://doi.org/10.12799/rcphn.2023.00241
Published online: December 29, 2023
1Epidemiological investigation officers, Incheon Airport National Quarantine Station, Korea Centers for Disease Control and Prevention(KDCA), Incheon, Korea
2Assistant professor, Department of Nursing Science, JEI University, Incheon, Korea
- Corresponding author: Yeom, Gye Jeong Department of Nursing, JEI University, 178, Jaeneung-ro, Dong-gu, Incheon 22573, Korea Tel: +82-32-890-7329, Fax: +82-32-890-7199, E-mail: salt42@hanmail.net
Copyright © 2023 Korean Academy of Community Health Nursing
This is an Open Access article distributed under the terms of the Creative Commons Attribution NoDerivs License. (http://creativecommons.org/licenses/by-nd/4.0) which allows readers to disseminate and reuse the article, as well as share and reuse the scientific material. It does not permit the creation of derivative works without specific permission.
- 1,015 Views
- 31 Download
Abstract
-
Purpose
- This study aimed to develop a simulation-based education program of emerging respiratory infectious diseases using standardized patients for nursing students, and to test the effects on basic epidemiological investigation performed while wearing Level D Personal Protective Equipment (PPE).
-
Methods
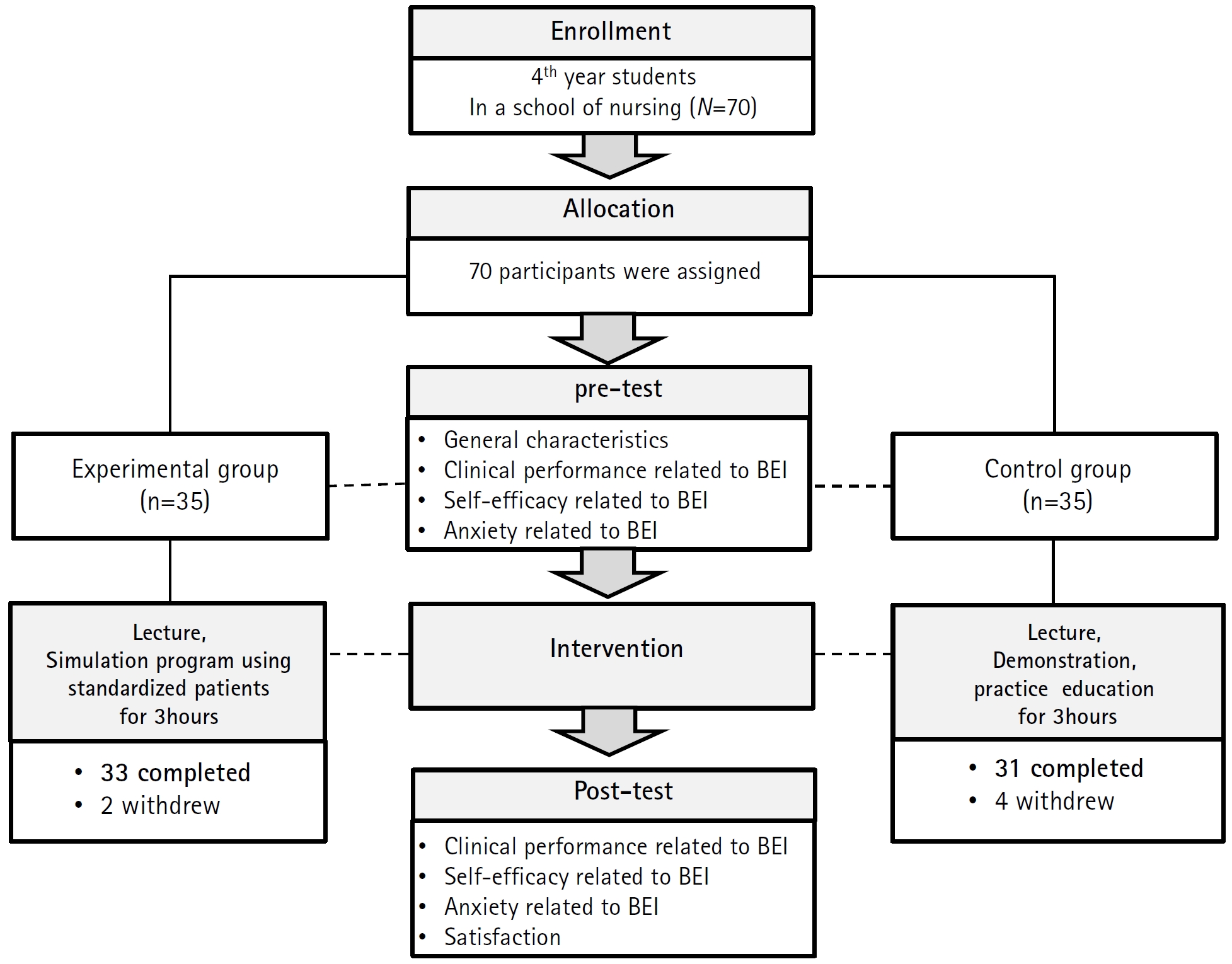
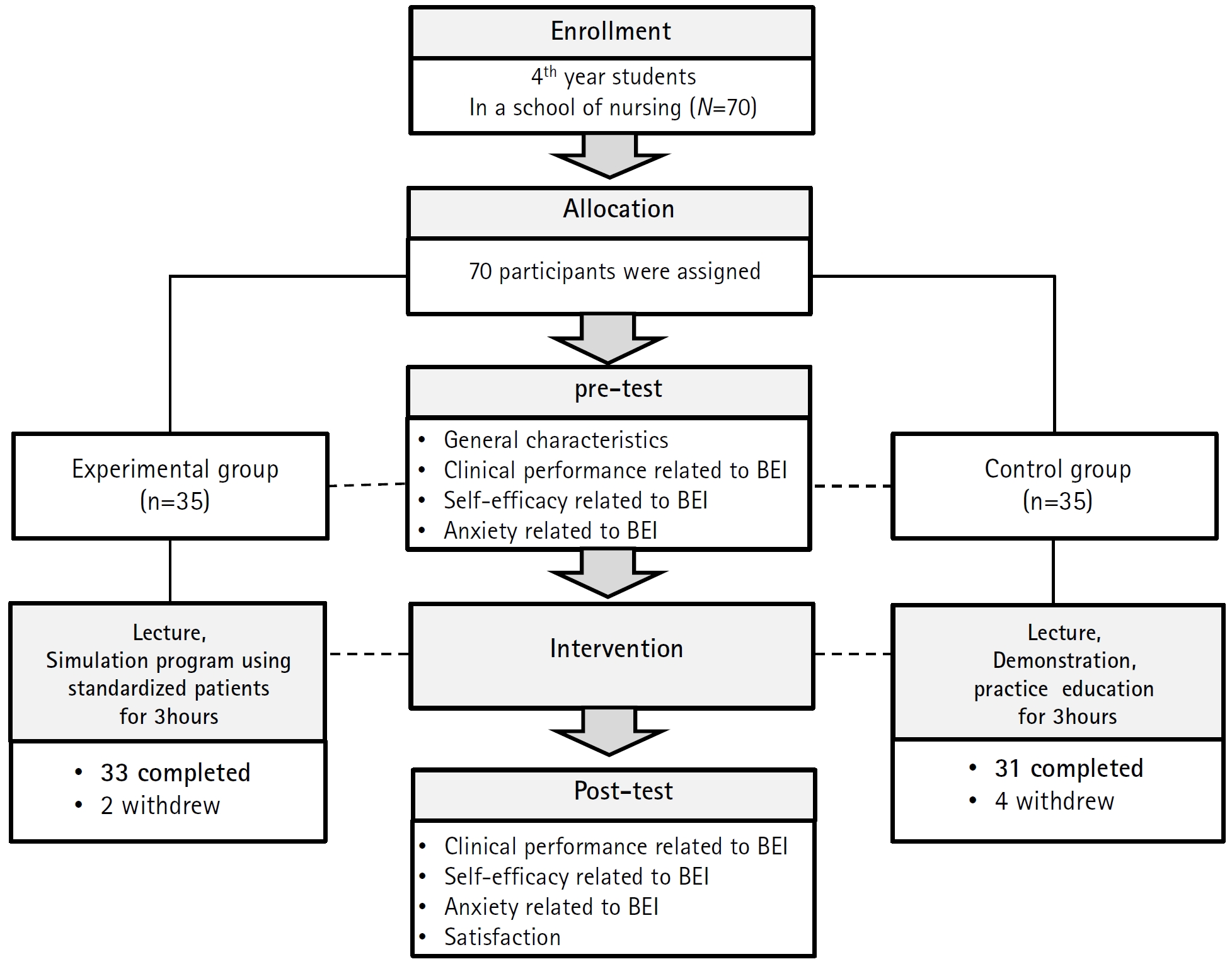
- A total of 64 senior nursing students were recruited and assigned to either the experimental group (n=33) or a control group (n=31) in May 2022. This program was developed based on the analysis, design, development, implementation, and evaluation model. The analysis phase consisted of a literature review and target group survey. In addition, learning objectives and a structure were designed, and a scenario was developed with expert consulting. In the implementation phase, the program was conducted the course of 3 hours. The evaluation phase involved verification of the effects on clinical performance, self-efficacy, and anxiety related to basic epidemiological investigation, as well as an assessment of satisfaction with the program.
-
Results
- There were significant differences between the experimental and control groups in clinical performance (z=-2.15, p=.010) and anxiety related to basic epidemiological investigation (z=-4.02, p<.001). However, there was no significant difference in self-efficacy related to basic epidemiological investigation.
-
Conclusion
- The results indicate that this simulation-based education program was effective in improving clinical performance and reducing anxiety related to basic epidemiological investigation of nursing students. In addition, this program is expected to be widely used as an epidemiological investigation education for the initial prevention of infectious diseases.
- Infectious diseases are a kind of social disaster, and disaster management regarding infectious diseases is being implemented at a national level [1]. In addition, a systematic management system for infectious diseases has been established and operated to prevent the outbreak and spread of infectious diseases [1]. When a public health crisis due to infectious diseases occurs, it is necessary to take appropriate measures to prevent the spread of infectious diseases based on prompt epidemiological investigations and the identification of the causes [2,3]. In particular, since emerging respiratory infectious diseases may cause respiratory complications caused by new pathogens and have the possibility of group outbreaks, it is important to take early action to identify the cause through epidemiological investigations and prepare measures for responses to the epidemic risk and the occurrence of an epidemic [4,5].
- Epidemiological investigations refer to activities for identifying the scale of the outbreak and tracing the source of infections to prevent the occurrence and spread of infectious diseases when patients with infectious diseases are found [6]. To perform these epidemiological investigations, professional workforce such as infectious disease specialist and epidemiological investigation officers are essentially required [7-9]. Basic epidemiological investigations are conducted through phone calls and interviews, and they include the examination of travel history about the outbreak areas, the epidemiological association of the presumed infection route, and clinical symptoms, and the investigation of contacts based on personal statements in addition to the examination of the personal information of persons under investigation. Each guideline of emerging infectious diseases includes a basic epidemiological investigation report form that enables the classification of cases for the diagnosis and reporting of cases according to the definitions of cases of infectious diseases. On the other hand, an in-depth epidemiological investigation involves activities such as checking whether the results of basic epidemiological investigations are correct or there is any missing information, cross interviews with contacts, and the identification of the source and route of infections by the investigation through the Epidemiological Investigation Support System (EISS) [10]. As described above, a basic epidemiological investigation is the stage for presenting criteria for testing prior to diagnostic tests, detecting suspected cases at an early stage, and reporting them, and it is an activity that requires various capabilities such as clinical decision making, communication, and disaster management. Also, it is an important part of the initial response for preventing the spread of infectious diseases in a disaster crisis situation arising from the outbreak of infectious diseases, and it is also a component of performance that nurses must have when they work in accordance with the temporary duty order under the Infectious Disease Control and Prevention Act [11-14].
- Simulation education is an educational method that integrates theoretical knowledge and practical coping abilities through the use of equipment and role play in safe virtual situations similar to actual situations, and it has been shown to improve coping capacity and practical competence in disaster nursing education including responses to the outbreaks of infectious diseases [15-18]. In particular, with respect to basic epidemiological investigation competency required to assess and appropriately respond to the suspected cases of infectious diseases, it has been reported that a better ability to effectively interact with persons under investigation and a higher level of self-efficacy were linked to a lower level of anxiety about infection control, and as a result, they were also associated with a higher level of clinical performance competency [7,17,19]. Thus, there is a need to develop and apply educational methods for improving the ability to perform basic epidemiological investigations by implementing simulation education that allows participants to apply knowledge and skills in safe virtual situations from the stage of education for undergraduate students [14,20]. In addition, it is necessary to apply educational methods using verbal and non-verbal expressions through standardized patients in relation to epidemiological relatedness and clinical symptoms in the implementation of basic epidemiological investigations that inevitably need to rely on the statements of persons under investigation. However, a review of the previous studies that conducted a systematic literature review on disaster education for nursing students [14,21,22] showed that there has not been sufficient research on interventions for strengthening the ability to perform basic epidemiological investigations for the early detection of suspected of contracting infectious disease in relation to responses to infectious disease disasters.
- Therefore, this study attempted to develop a scenario on the basic epidemiological investigations of emerging respiratory infectious diseases for nursing students, and examine the effects of simulation education using standardized patients (SPs) on clinical performance, self-efficacy, and anxiety related to basic epidemiological investigations among nursing students with the aim of providing a simulation education program that can be utilized as an educational material on the basic epidemiological investigations of emerging respiratory infectious diseases for nursing students.
- Objectives
- This study aimed to develop and apply a simulation education program using standardized patients on basic epidemiological investigations regarding emerging respiratory infectious diseases, and investigate the effects of the developed program on clinical performance, self-efficacy, and anxiety among nursing students. The specific objectives of this study are as follows.
- 1) To develop a simulation education program using standardized patients on the basic epidemiological investigations of emerging respiratory infectious diseases;
- 2) To examine the effects of a simulation education program on basic epidemiological investigations using standardized patients on clinical performance, self-efficacy, and anxiety related to basic epidemiological investigations among nursing students.
- Research hypotheses
- H1. The experimental group that received simulation education on basic epidemiological investigations using standardized patients will show a greater improvement in clinical performance related to basic epidemiological investigations than the control group.
- H2. The experimental group that received simulation education on basic epidemiological investigations using standardized patients will show a greater improvement in self-efficacy related to basic epidemiological investigations than the control group.
- H3. The experimental group that received simulation education on basic epidemiological investigations using standardized patients will show a greater decrease in anxiety related to basic epidemiological investigations than the control group.
Introduction
- 1. Study design
- This study is a quasi-experimental research using a non-equivalent control group pretest-posttest design, and this research was conducted to develop and apply a simulation education program using standardized patients on the basic epidemiological investigations of emerging respiratory infectious diseases, and verify the effectiveness of the developed simulation education program.
- 2. Participants
- The participants of this study were nursing students attending a university in Incheon, and they were selected through an open recruitment from the senior students who took a community nursing course. After providing sufficient explanations about this study to the eligible students, only persons who understood the purpose of the study and voluntarily agreed to participate in the study were recruited. For the voluntary participation of students, participants were recruited by the researcher, who was not a faculty member of the university. The sample size was calculated using the G*power 3.1.9.7 Version, and the minimum sample size was determined as 26 persons per group by using a significance level of .05, an effect size of .80, and a power of .80. Considering the dropout rate, 35 persons for each group were recruited by convenience sampling. Afterwards, 6 persons withdrew from this research during the intervention period because they were absent from education due to their job interviews. Finally, 33 persons in the experimental group participated in simulation education using standardized patients, and 31 persons in the control participated in demonstrations and simple practice training. As a result, the data collected from a total of 64 participants were used for analysis (Figure 1).
- 3. Development procedure
- In this study, the development of the simulation education program was carried out, based on the ADDIE instructional design model comprised of 5 phases: Analysis, Design, Development, Implementation, and Evaluation [23].
- A review of recent domestic and foreign studies was conducted to identify research trends and educational needs regarding education on infectious diseases and disaster education. This review of previous studies showed that there is a need to provide nurses with education for strengthening the disaster coping capacity from the stage of undergraduate education in order for nurses to have the capacity to play a central role in disaster crisis situations [14,20,21]. In addition, it was found that simulation education is recommended as an educational method that can complement clinical practice since it allows repetitive practice in a safe educational environment similar to clinical settings, and that there is a need to apply simulation education as a method to enhance nursing students’ basic epidemiological investigation competency related to the outbreaks of infectious diseases, and examine the effects of simulation education [15-18].
- To select the education topic of the scenario of simulation education, previous studies on education on infection control and disaster responses for healthcare professionals after the outbreak of COVID-19 [24-26] were examined, and the interview with the expert focus group consisting of two epidemiological investigation officers and two nursing professors as well as interviews with 5 nursing students were performed. As a result, case classification and responses regarding emerging infectious diseases through basic epidemiological investigations including the epidemiological investigations of infectious diseases and the methods of donning and doffing personal protective equipment (PPE) were selected as the education topic.
- Based on Bloom’s taxonomy, educational objectives were determined as follows: the cognitive objective was set as being able to explain the basic principles of infection control of medical institutions, the affective objective was set as being able to classify patients according to case definitions, and the psychomotor objectives were set as being able to provide appropriate information to suspected of contracting infectious disease (including patients under investigation, PUI) and being able to have therapeutic communication with patients [27].
- In this study, the content of theoretical education was composed of criteria for the classification of infectious diseases in accordance with the Infectious Disease Control and Prevention Act, rational bases for epidemiological investigations, the method of epidemiological investigations, the method of donning and doffing personal protective equipment (PPE), an overview of negative pressure isolation rooms, and environment and waste management. The simulation scenario was created as a hypothetical situation where a basic epidemiological investigation is conducted on hypothetically posited cases of an imported emerging infectious disease (tentatively called Indian flu), and the scenario included case classification according to the guidelines for responses to the outbreak of a Group 1 emerging infectious disease and the reporting and quarantine of patients under investigation immediately after the classification of cases into suspected of contracting infectious disease. The content of the education program was designed based on guidelines for responses to emerging respiratory infectious diseases, guidelines for isolation precautions for medical institutions, standards of ventilation for medical facilities, standards of personal protective equipment (PPE), and the information material on the methods of donning and doffing PPE (level D) distributed by the Korea Disease Control and Prevention Agency [28-31].
- The total education time for the education program developed in this study is 3 hours, and it includes 15 minutes for orientation, 60 minutes for theoretical education prior to simulation education, 15 minutes for pre-briefing, 30 minutes for the operation of BEI simulation including donning and doffing PPE, and 30 minutes for debriefing. The participants were divided into four-member teams, and they were given explanations about the simulated situation, the first and final steps of the simulation, the movement path, and preparation items during pre-briefing. As for the standardized patient (SP), a person who completed the SP training course, and received prior training regarding the scenario of this study performed the role of a suspected of contracting infectious disease. Simulation starts with putting on personal protective equipment (PPE) in the anteroom, and, as the next step, an epidemiological investigation with the patient under investigation is performed in the screening room. The simulation process is finished when education participants take off PPE after guiding the suspected of contracting infectious disease into the negative pressure isolation room following case classification. A part of the simulation area was designated as the negative pressure isolation room by dividing the space by using curtains and positing a sign indicating the negative pressure isolation room, and to visually check the performance of donning and doffing PPE, florescent lotion was applied after putting on PPE, the remaining florescent lotion was examined after taking off PPE. Based on the Gather-Analyze-Summarize (GAS), the debriefing process was composed of three steps: description, analysis, and application [32, 33]. The details of the BEI simulation education program developed by this study are presented in Table 1. On the other hand, the practice training of the control group consisted of completing a BEI form through a team learning process according to the scenario and performing case classification according to case definitions. In additions, the participants in the control group also performed donning and doffing PPE, but the education program for the control group did not include the process of checking florescent material unlike the program of the experimental group.
- Satisfaction with the education program was assessed immediately after the completion of simulation education by using a tool developed by Yoo [34], which was composed of 24 questions. The assessment of learners’ satisfaction was designed to make it possible to obtain detailed feedback through open-ended questions and interviews.
- The case of the scenario was hypothetically posited through the researcher’s modification and supplementation of the situation of reported cases of COVID-19, based on the imported confirmed cases of COVID-19. To reproduce the situation of an epidemiological investigation performed by making an inquiry with a suspected of contracting infectious disease, verbal and nonverbal expressions were used by applying standardized patients. The BEI form was created as a form suitable for the hypothetical case of an emerging respiratory infectious disease (tentatively referred to as Indian flu) by modifying and complementing the BEI form for COVID-19 to make it suitable for the cases of a hypothetical emerging respiratory infectious disease presented in the scenario. The design of the scenario was conducted using the scenario composition template that is used at C University in Seoul. This module includes the simulation topic, class operation, scenario situations (for professors, for students, and for SPs), BEI forms (for students and for SPs), training scripts for standardized patients (SPs), and the debriefing plan. In addition, guidelines on responses to emerging respiratory infectious diseases were created in consideration of the situation of the scenario developed in this study in order to lead participants to perform case classification and patient isolation after conducting basic epidemiological investigations regarding suspected cases. The researcher is currently working as an epidemiological investigation officer of a national government institution, majored in simulation, and completed courses on simulation teaching methods, simulation operation, and SP education and training as part of the doctoral program in order to prepare in advance for this research.
- The verification of content validity of the developed simulation education program on the basic epidemiological investigations of emerging respiratory infectious diseases was performed through the analysis of the content validity index (CVI). This verification of content validity was performed by six experts, and they consisted of an infection control nurse, an officer of a national government institution, two epidemiological investigation officers of local governments, and two nursing professors. The content validity of each item was measured on a 4-point Likert scale ranging from 1 point (= ‘Not valid at all’) to 4 points (= ‘Very valid’), and the CVI of this study was 0.9~1.0. Based on the feedback that the time for scenario operation would be insufficient among experts’ comments, the final scenario was completed by removing the processes of selecting PPE and reporting the infectious disease.
- Prior to implementation, a preliminary experiment on the developed simulation education on basic epidemiological investigations of emerging respiratory infectious diseases was conducted in C University located in Seoul for 3 days from April 27 to 29, 2022. A total of 13 participants were recruited, and they were divided into 3 teams.
- After the completion of education, the comparison of the levels of satisfaction with education between the experimental and control groups was made. The level of satisfaction with education was 4.85±0.30 points out of 5 in the experimental group, and 4.58±0.32 points in the control group (t=-3.54, p<.001). Specifically, the feedback obtained through open-ended questions and interviews included the following opinions: ‘The application of standardized patients made me feel like it was a real situation’; ‘I found it useful to have the opportunity to trace epidemiological relatedness through debriefing’; ‘Actually donning PPE and checking it through florescent lotion led me to think that I need to be more careful’; ‘Through discussion and reflection during debriefing, I realized that it is also necessary to pay attention to the non-verbal expressions of standardize patients.’ Regarding aspects that need to be improved, the following suggestions were given: ‘It would be better if students are given an opportunity to introduce themselves to each other as well as a longer break and a sufficient time to prepare for the next class.’ In addition, the instructor performed the overall evaluation about the levels of accomplishment of educational objectives, time management, and problems in the process of proceeding with education according to the scenario. The results of evaluation of the effectiveness of simulation education are described in the section about the verification of effectiveness.
- 4. Measures
- The assessment tool for clinical performance related to basic epidemiological investigations (BEI) was developed by the researcher in the design phase. This scale contains a total of 40 questions, and it is composed of questions on five subdomains of clinical performance as follows: 12 questions on donning PPE, 12 questions on basic epidemiological investigations, 3 questions on the isolation of suspected patients, 10 questions on doffing PPE, and 3 questions on environment and waste management. Regarding the content validity of the developed questions and the categorization of them, the analysis of CVI by 6 experts was conducted, and the six experts consisted of an infection control nurse, an epidemiological investigation officer of a national government institution, two epidemiological investigation officers of local governments, and two nursing professors. Then, the questions were finally selected through face validity analysis in the evaluation stage. Regarding the reliability of the tool, the value of Cronbach's α was calculated as .97.
- Self-efficacy related to basic epidemiological investigations was measured using a modified version of the self-efficacy scale used by Jung [36]. Jung [36] developed a Korean modified version of the scale developed by Sherer et al. [35] by revising and complementing the original tool. The tool used in this study was created by the researcher by remodifying the version created by Jung [36] to make it suitable for basic epidemiological investigations, and this scale consists of a total of 17 questions. Each item is assessed on a 5-point Likert scale ranging from 1 point (=‘Not confident at all’) to 5 points (= ‘Very confident’). Higher scores indicate higher levels of self-efficacy. As for the reliability of the tool, the value of Cronbach's α of the original tool was reported as .86, and the value of Cronbach's α was calculated as .94 in this study.
- Anxiety related to the performance of basic epidemiological investigations was measured using a modified version of the infection-related anxiety assessment tool presented by Kim et al. [19]. The modified version used in this study was created by the researcher by modifying and complementing the original tool in consideration of the content of the performance of basic epidemiological investigations and exposure to the risk for infection in the process. The content validity of the used instrument was confirmed though the verification of experts. Higher scores indicate higher levels of anxiety. The scale used consists of 4 questions, and each item is rated on a 10-point numeric rating scale (0 points: ‘Not anxious at all’; 5 points: ‘Moderately anxious’; 10 points: ‘Very anxious’). The value of Cronbach's was reported as α .97 by the creator of the tool, and it was calculated as .89 in this study.
- 5. Data collection
- Data was collected from May 1 to 20, 2022. The education program was carried out by assigning 16~17 students per session, so a total of four sessions were delivered by performing two sessions for each group. To block the ripple (imitation) effect among participants, the education sessions of experimental and control groups were performed separately on different dates, and participants were not informed in advance about which group they were assigned to. A pre-survey was conducted using a structured self-administered questionnaire among the students who voluntarily agreed to participate the day before the implementation of the education program, and a post-survey was conducted immediately after the completion of the education program. For fairness, the control group that participated in demonstrations and simple practice training was also given simulation education after the post-test survey. In addition, it was explained to the students that the education program and surveys related to this study were all conducted for the purpose of research, and they were not related to the marks or grades of college courses or the evaluation of practice education.
- 6. Data analysis
- The collected data was analyzed using SPSS Statistics 26.0. As a result of conducting the Shapiro-Wilk test prior to analysis, the p-value for the dependent variable was calculated as less than .05, so analysis was conducted using nonparametric tests. The preliminary test of the homogeneity of two groups was performed using the Chi-squared test and the Mann Whitney U test. To test hypotheses, the Wilcoxon singled-rank test was used for the within-group comparison and the Mann Whitney U test was used for testing for differences between two groups.
- 7. Ethical considerations
- For the ethical protection of the rights of participants, this study was conducted after obtaining approval from the Institutional Review Board of Chung-Ang University (IRB No. 1041078-202201-HR-029). The voluntary participation of study participants, the protection of anonymity and confidentiality, possibility of withdrawal from research, and no disadvantages and no harm arising from research were specified in the participation information sheet, and written informed consent was obtained from participants after explaining the content of the participation information sheet to them.
Methods
1) Analysis phase
(1) Data collection through a literature review
(2) Examination and selection of learners’ educational needs
2) Design phase
(1) Setting and specification of educational objectives
(2) Design of educational content and operation methods
(3) Design of the education evaluation tool
3) Development phase
(1) Development of the scenario about an emerging respiratory infectious disease
(2) Expert consultation and verification of content validity
4) Implementation phase
5) Evaluation phase
1) Clinical performance related to basic epidemiological investigations
2) Self-efficacy related to basic epidemiological investigations
3) Anxiety related to basic epidemiological investigations
- 1. Verification of the homogeneity of participants
- To verify the homogeneity of two groups for general characteristics, the comparison of age (Z=13.45, p= .265), gender (χ2=0.27, p= .603), the number of the experience of participation in simulation education (χ2=2.19, p=.140), and academic performance (χ2=0.02, p= .877) were conducted, and it was found that there were no significant differences. In addition, to examine the homogeneity of the values of research variables prior to the intervention, the comparison of clinical performance related to BEI (Z=45.98, p= .473), self-efficacy related to BEI (Z=35.14, p= .462), and anxiety related to BEI (Z=14.65, p= .840) between two groups was conducted, and the results showed that there were no significant differences (Table 2).
- 2. Verification of hypotheses
- In this study, Hypothesis 1 was postulated as follows: The experimental group that received BEI simulation education using standardized patients will show a greater improvement in clinical performance related to basic epidemiological investigations than the control group. The results of data analysis revealed that the score for clinical performance related to BEI was increased by 2.15 points (1.75~2.86) in the experimental group and by 1.63 points (1.33~2.13) in the control group after education, compared to the pre-intervention scores. The analysis for significance of differences between the two groups revealed that there were significant differences between the two groups, so Hypothesis 1 was supported. Regarding the sub factors of clinical performance, there were significant differences between two groups in donning PPE (Z=-2.14, p= .033), basic epidemiological investigation (Z=-2.80, p= .005), and environment and waste management (Z=-2.74, p=.006), but there was no statistically significant difference between two groups in the isolation of suspected patients (Z=-1.51, p=.131) and doffing PPE (Z=-1.78, p=.075) (Table 3).
- Analysis of the collected data was conducted to test the Hypothesis 2 that the experimental group that received BEI simulation education using standardized patients will show a greater improvement in self-efficacy related to basic epidemiological investigations than the control group. The analysis results showed that the score for self-efficacy related to basic epidemiological investigations was increased by 1.76 points (1.03~2.44) in the experimental group and by 1.53 points (1.00~2.06) in the control group, but there was no significant difference between the two groups (Z=-0.79, p= .432). As a result, Hypothesis 2 was not supported (Table 3).
- In this study, Hypothesis 3 was postulated as follows: The experimental group that received BEI simulation education using standardized patients will show a greater decrease in anxiety related to the clinical performance of basic epidemiological investigations than the control group. The results of analysis of the collected data revealed that the score for anxiety was decreased by 18.00 points on average (-23.00~-13.50) in the experimental group and by 10.00 points on average (-16.00~-6.00) in the control group after education, compared to the pre-intervention scores, and there was a significant difference between two groups (Z=-4.02, p< .001). In other words, the results of this study supported Hypothesis 3. Regarding the sub factors of anxiety, there were significant differences in all of the following sub factors of anxiety: anxiety about infection due to contact with suspected patients (Z=-4.45, p< .001), anxiety about the performance of basic epidemiological investigations (Z=-3.92, p< .001), anxiety about infection due to donning and doffing PPE (Z=-2.95, p= .003), and anxiety about infection due to environment management and medical waste disposal (Z=-2.41, p= .016) (Table 3).
Results
1) Verification of Hypothesis 1
2) Verification of Hypothesis 2.
3) Verification of Hypothesis 3
- This study developed and applied a simulation education program on the basic epidemiological investigations (BEI) of emerging respiratory infectious diseases for nursing students to improve BEI performance competency and effective prepare for responses to disasters and crises due to the outbreak of infectious diseases and verified the effectiveness of the developed simulation education among nursing students. In this study, the development of simulation education was carried out according to the ADDIE instructional design model by systematically developing a scenario and subsequently operating the simulation education program. This simulation education made it possible to realistically reproduce social disaster situations such as the outbreak of infectious diseases, which are difficult to reproduce in existing demonstrations and simple practice education. In particular, the simulation education program developed in this study reflected nursing students’ educational needs regarding education on infection control by including donning and doffing PPE and the performance of patient isolation in addition to basic epidemiological investigations. Therefore, this simulation education program can be utilized for the enhancement of both BEI competency and infection control competency needed for initial infection control measures in the case of disaster and crisis responses.
- The analysis of the effects of simulation education developed in this study revealed that the experimental group showed a greater improvement in clinical performance related to BEI than the control group. These results are consistent with the previous studies that reported that simulation education resulted in significant differences in clinical performance between groups [19,21,37]. In particular, this study increased the fidelity of simulation education by applying standardized patients in basic epidemiological investigations, which inevitably rely on the statements of patients under investigation, and provided an environment similar to clinical settings, and these factors are thought to have contributed to the improvement of clinical performance in the experimental group.
- Meanwhile, in this study, the level of self-efficacy related to BEI was increased in both groups after education, compared to the pre-intervention scores, and there was no significant difference between two groups. These results are in agreement with the findings of Kim et al. [19]. In a prior study by Kim et al. [19], the experimental group participated in an infection control education program using SP, while the control group participated in peer role-play practice. In this study, the lack of significant differences in self-efficacy between two groups is presumed to be related to the team-based practice of the control group. More specifically, when the control group performed the simple practice about completing BEI forms about the cases presented to them, the participants of the control group were divided into teams with 4-5 members. This team-based practice is presumed to have induced cooperative learning among peers and have contributed to the increase of self-efficacy for BEI. Actually, in this study, the mean scores for self-efficacy related to BEI in the experimental and control groups were 4.71 points and 4.59 points out of 5, respectively, and these scores are relatively higher than the mean scores of 3.52~3.56 points reported in previous studies [38, 39]. Therefore, there is a need to consider education programs including peer-led debriefing and team debriefing to promote cooperation in the learning process in the future development of simulation education programs.
- In this study, although both groups showed a significant decrease in the level of anxiety related to BEI after education, compared to pre-intervention survey results, the experimental group showed a greater decrease in the level of anxiety, and there was a significant difference between two groups. These results are consistent with the previous studies that reported a reduction in anxiety after simulation education [15, 19]. In the experimental group, among the sub factors of anxiety, anxiety about infection due to contact with suspected patients showed the greatest reduction. This greater decrease in anxiety about contact with suspected patients in the experimental group is thought to be related to the specific method of simulation applied to the experimental group. In other words, participants in the experimental group performed a face-to-face assessment of the SP by wearing PPE prior to the patient assessment, and their simulation included the process of checking the florescent material after doffing PPE. The results about anxiety reduction through simulation education are consistent with the findings of Yoo [40]. In a study of nursing students’ educational needs regarding education on infection control, Yoo [40] reported that nursing students were found to have the highest educational need for the domain of the importance and performance of donning and doffing Level D PPE. The results about anxiety of this study are also in agreement with the findings of Ji and Seo [41]. Ji and Seo [41] conducted research on simulation education using SP about nursing care of patients on contact precautions, and reported that simulation education performed by wearing PPE showed satisfactory educational effects in terms of contact with actual people and the performance of nursing care of patients on contact precautions. On the other hand, in a study conducted before the outbreak of COVID-19, Kim et al. [19] reported that simulation education on infection control did not lead to any significant changes in anxiety about contact with patients with respiratory infectious diseases as a sub factor of anxiety after. The study results of Kim et al. [19] may be attributed to the following reason. It seems that since only an N95 mask and gloves were worn as PPE during simulation in the study, the simulation was not effective in the reduction of anxiety related to contact with patients with respiratory infectious diseases. Due to the recent COVID-19 pandemic, there is an increased need for education on the nursing of patients with emerging respiratory infectious diseases, and this study developed and applied simulation education tailored to the educational needs of nurses such as the method of donning and doffing personal protective equipment. In view of the results of this study and the current situation, there is a need for further research to develop various scenarios by reflecting the social changes and educational needs of nurses.
- In the evaluation phase after the completion of education programs, simulation education was found to have an effect on satisfaction with education. The significantly higher level of satisfaction with education in the experimental group may be attributed to the following reasons. First, the need for education on the method of epidemiological investigations and infection control has been increased in nursing students due to the recent COVID-19 pandemic situation [40]. In addition, participants participated in simulation education wearing PPE by applying standardized patients, and this application of standardized patients made them feel like they were in a real situation. In particular, while participants in the control group immediately presented epidemiological relatedness (contact with a confirmed patient) and clinical symptoms, those in the experimental group experienced nonverbal expressions as well as the investigation process including the examination of the incubation period and checking the epidemiological association with standardized patients, and they had the opportunity for reflection through debriefing. The responses to open-ended questions among the survey items showed that the above-mentioned processes in the experimental group increased the level of satisfaction of learners. In this respect, it is considered meaningful that this study induced reflection through systematic and structured debriefing. In the future, there is a need for instructors to lead a stepwise analysis by varying the level of reflection facilitation depending on the degree of immersion in debriefing among participants who do not have the previous experience of simulation education.
- In a previous study on infection control education for nurses, Yang [17] conducted research on education for the nurses of medical institutions regarding writing BEI forms and the subsequent measures such as the isolation of patients, testing, and environment management, and this prior study was focused on education for the control of further infectious disease spread at the stage of the community spread of an infectious disease. In contrast, this study conducted research on education on the importance of community nurses’ initial basic epidemiological investigations by comprehensively checking the stages and guidelines of the crisis warning system regarding infectious diseases and performing case classification in a situation where the transmission of emerging respiratory infectious diseases does not occur in Korea. The BEI of emerging respiratory infectious diseases is one of initial infection control and prevention measures, and it is an important step for the early detection of suspected patients and the prevention of further spread or outbreaks by investigating the epidemiological relatedness and clinical symptoms in compliance with guidelines changed according to the situation of outbreaks of infectious diseases and the results of epidemiological investigations from the beginning of the occurrence of emerging infectious diseases. Nurses and students must be equipped with capabilities and expertise through crisis response training and the process of responding to infectious diseases in normal times in preparation for disasters. Also, this education on infection control and how to respond to infections should be carried out through participatory simulations rather than lecture-based education, and lead students to learn a series of processes in which they recognize and report problems, perform necessary actions, and resolve problems about patients on their own [41].However, since nursing students may be exposed to danger in the process of participating in practice training in actual clinical situations, this study attempted to provide a safe simulation environment for nursing students and integrate knowledge and skills related to basic epidemiological investigations. This study also developed and applied an education program based on the guidelines and cases of emerging infectious diseases, and the education program developed by this study will hopefully contribute to the early detection of infectious diseases and the prevention of the spread of the diseases through the enhancement of BEI competency required to respond to disaster crises caused by emerging infectious diseases in the future.
Discussion
- This study developed a simulation education program on basic epidemiological investigations (BEI), based on the guidelines and cases of emerging respiratory infectious diseases, and this simulation education program includes the performance of BEI, donning and doffing PPE, and the isolation of suspected patients. To evaluate the effectiveness of the developed BEI simulation education program, this study operated the developed BEI simulation education program using standardized patients (SP), and assessed clinical performance related to BEI, self-efficacy related to BEI, and anxiety related to BEI in the experimental and control groups. As a result, simulation education using SP was found to be more effective in the improvement of clinical performance and the reduction of anxiety than education using only demonstrations or simple practice. If the simulation education program developed by this study is utilized for the improvement of BEI competency needed for responses to disaster crises due to emerging infectious diseases, it is expected to contribute to the early detection of infectious diseases and the prevention of their spread in the future. This study has limitations in generalizing research findings since participants were recruited only from nursing students attending a single university located in Incheon. Moreover, in this study, the clinical performance competency for BEI was assessed using a self-administered survey, so there is a need to objectively measure the clinical performance ability for BEI in actual healthcare settings. Based on the results of this study, simulation programs at various levels for learners such as nurses and epidemiological investigation officers should be developed, and there is also a need for replication studies to examine learning effects. In addition, further research should be conducted to evaluate the actual effectiveness of the developed simulation education program in terms of the control of infectious diseases through early infection control measures and the prevention of the spread of emerging infectious diseases after the implementation of the developed BEI simulation education program.
Conclusions
-
Conflict of interest
The authors declared no conflict of interest.
-
Funding
None.
-
Authors’ contributions
Park, Jiyun contributed to conceptualization, data curation, formal analysis, funding acquisition, methodology, project administration, visualization, writing-original draft, investigation, software, and supervision. Yeom, Gye Jeong contributed to writing – review & editing, resources, visualization, and validation.
-
Data availability
Please contact the corresponding author for data availability.
NOTES
Acknowledgments
- 1. Jeong EK. Public health emergency preparedness and response to emerging infectious diseases. Journal of the Korean Medical Association. 2017;60(4):296–299. http://doi.org/10.5124/jkma.2017.60.4.296Article
- 2. Tak SW. A review of the US public health emergency preparedness in the context of COVID-19. Global Social Security Review. 2020;13:5–20. https://doi.org/10.23063/2020.06.1Article
- 3. Lee MS, Kim EY, Lee SW. Experience of 16 years and its associated challenges in the Field Epidemiology Training Program in Korea. Epidemiology and Health. 2017;39:e2017058. https://doi.org/10.4178/epih.e2017058ArticlePubMedPMC
- 4. Kim NS. Current status and challenges of COVID-19. Issue & Focus. 2020;373:1–13. http://doi.org/10.23064/2020.03.373Article
- 5. Song SH, Choi JK, Kim SR. Response system for emerging infectious disease crisis - Focusing on the organization and the operation of an initial response task force. Crisisonomy. 2020;16(5):1–16. https://doi.org/10.14251/crisisonomy.2020.16.5.1Article
- 6. National Law Information Center [Internet]. Infectious disease prevention and management act, hereinafter infectious disease prevention act. Act No. 18507. 2022 [cited 2023 July 1]. Available from: https://www.law.go.kr
- 7. Lee MS. Improvement of epidemiology intelligence service officer program for preparedness and response against future health issues included communicable and non-communicable diseases in Korea. Health Policy and Management. 2018;28(3):294–300. https://doi.org/10.4332/KJHPA.2018.28.3.294Article
- 8. Calisher C, Carroll D, Cowell R, Corley RB, Daszak P, Drosten C, et al. Statement in support of the scientists, public health professionals, and medical professionals of China combatting COVID-19. The Lancet. 2020;395(10226):e42–e43. https://doi.org/10.1016/S0140-6736(20)30418-9ArticlePubMed
- 9. Daly ER. A review of the applied epidemiology workforce in the United States: Past, present, and future. Annals of Epidemiology. 2021;58:94–103. https://doi.org/10.1016/j.annepidem.2021.03.002Article
- 10. Park MJ. Examination of the principle of proportionality for the COVID-19 contact tracing. Asia Pacific Journal of Health Law & Ethics. 2021;14(2):1–25. https://doi.org/10.38046/apjhle.2021.14.2.001Article
- 11. Bak JA, Choi SH. Roles of local governments and problems of the legal policy for the prevention and management of infectious diseases. Journal of Law and Politics Research. 2021;21(1):285–318. http://doi.org/10.17926/kaolp.2021.21.1.285Article
- 12. Son HM, Yang HR, Park BH. Experiences of public officials for the COVID-19 response in the community health center. Research in Community and Public Health Nursing. 2021;32(4):578–592. https://doi.org/10.12799/jkachn.2021.32.4.578Article
- 13. Goni-Fuste B, Wennberg L, Martin-Delgado L, Alfonso-Arias C, Martin-Ferreres ML, Monforte-Royo C. Experiences and needs of nursing students during pandemic outbreaks: A systematic overview of the literature. Journal of Professional Nursing. 2021;37(1):53–64. https://doi.org/10.1016/j.profnurs.2020.12.004ArticlePubMedPMC
- 14. Loke AY, Guo C, Molassiotis A. Development of disaster nursing education and training programs in the past 20 years (2000–2019): A systematic review. Nurse Education Today. 2021;99:104809. https://doi.org/10.1016/j.nedt.2021.104809ArticlePubMed
- 15. Yoo EY, Jung YK. Training effectiveness of the COVID-19 infection control simulation program on nursing students. The Journal of Humanities and Social Science. 2020;11(6):939–954. http://doi.org/10.22143/HSS21.11.6.66Article
- 16. Kim HJ, Lee SH. Experience of clinical simulation practice through map training based on infectious disease occurrence scenarios of nursing college students. The Journal of Learner-Centered Curriculum and Instruction. 2021;21(16):39–54. https://doi.org/10.22251/jlcci.2021.21.16.39Article
- 17. Yang SH. The effect of new respiratory infectious disease simulation education on knowledge, clinical performance and self-efficacy of emergency room nurses [master’s thesis]. [Nonsan]: Konyang University; 2021. 69 p.
- 18. Dieckmann P, Torgeirsen K, Qvindesland SA, Thomas L, Bushell V, Ersdal HL. The use of simulation to prepare and improve responses to infectious disease outbreaks like COVID-19: Practical tips and resources from Norway, Denmark, and the UK. Advances in Simulation. 2020;5(1):1–10. https://doi.org/10.1186/s41077-020-00121-5ArticlePubMedPMC
- 19. Kim EY, Kim SS, Kim SH. Effects of infection control education for nursing students using standardized patients vs. Peer role-play. International Journal of Environmental Research and Public Health. 2021;18(1):107. https://doi.org/10.3390/ijerph18010107ArticlePubMedPMC
- 20. Kang JY. Simulated nursing practice education in the ontact age: A mixed methods case study. The Journal of Learner-Centered Curriculum and Instruction. 2020;20(18):937–957. http://doi.org/10.22251/jlcci.2020.20.18.937Article
- 21. Hong EJ. A literature review of studies on disaster training for nursing students and nurses. Journal of Convergence for Information Technology. 2020;10(5):60–74. https://doi.org/10.22156/CS4SMB.2020.10.05.060Article
- 22. Kim SH, Kim HJ. Simulation-based disaster nursing education program for nursing student: A systematic review. Journal of Korea Society for Simulation in Nursing. 2021;9(1):69–87. http://doi.org/10.17333/JKSSN.2021.9.1.69Article
- 23. Dick W, Carey L, Carey JO. Systematic design of instruction. 7th ed. New Jersey: Pearson College Div; 2008. 396 p.
- 24. Rim DH, Shin HS, Jeon HJ, Kim JE, Chun HJ, Oh H, et al. Collaborative disaster governance recognized by nurses during a pandemic. Journal of Korean Academyof Nursing. 2021;51(6):703–719. https://doi.org/10.4040/jkan.21163ArticlePubMed
- 25. Choi MJ, Jeong HS, Joung YS, Lee HY. Analysis of needs for infection control education in long-term care hospitals for the epidemic of COVID-19: Borich priority formula and the locus for focus model. Health and Social Welfare Review. 2021;41(1):8–21. http://doi.org/10.15709/hswr.2021.41.1.8Article
- 26. Oh EG. Perspectives on nursing profession for a post-COVID-19 new normal. Korean Journal of Adult Nursing. 2020;32(3):221–222. https://doi.org/10.7475/kjan.2020.32.3.221Article
- 27. Bloom BS. Taxonomy of educational objectives. HandbookⅠ: Cognitive Domain. New York: David Mckay; 1956. 207 p.
- 28. Korea Disease Control and Prevention Agency. Emerging respiratory infectious disease response guidelines [Internet]. Cheongju: Korea Disease Control and Prevention Agency. 2022 [cited 2023 Jul 1]. Available from: https://www.kdca.go.kr/
- 29. Hospital Nurses Association. Guideline for isolation precautions in healthcare settings [Internet]. Seoul: Hospital Nurses Association. 2016 [cited 2023 Jul 1]. Available from: https://khna.or.kr/
- 30. Seong MG. COVID-19 management in healthcare facilities -ventilation standards and challenges. Air Cleaning Technology. 2021;34(2):14–24.
- 31. National Institute for Occupational Safety and Health. Guidance on emergency responder personal protective equipment (PPE) for response to CBRN terrorism incidents [Internet]. Washington, DC: NIOSH-Issued Publications. 2008 [cited 2014 Jun 6]. Available from: https://www.cdc.gov/niosh/docs/2008-132/
- 32. Paul EP, John MO. Debriefing using a structured and supported approach. In: Adam IL, Samuel D, Andrew DS, Alan JS, editors. The comprehensive textbook of healthcare simulation. New York: Springer; 2013. p. 73–84. https://doi.org/10.1007/978-1-4614-5993-4_6
- 33. Jaye P, Thomas L, Reedy G. 'The Diamond': A structure for simulation debrief. The Clinical Teacher. 2015;12(3):171–175. https://doi.org/10.1111/tct.12300ArticlePubMedPMC
- 34. Yoo MS. The effectiveness of standardized patient managed instruction for a fundamental nursing course. The Journal of Korean Academic Society of Nursing Education. 2001;7(1):94–112.
- 35. Sherer M, Adams CH. Construct validation of the self-efficacy scale. Psychological Reports. 1983;53(3):899–902. https://doi.org/10.2466/pr0.1983.53.3.899Article
- 36. Jung AS. A Study on the relations between a health promoting behaviors and self-efficacy in general hospital nurse [master’s thesis]. [Seoul]: Hanyang University; 2007. 68 p.
- 37. Kang H. The effects of simulation-based education on the clinical reasoning competence, clinical competence, and educational satisfaction. Journal of the Korea Academia-Industrial cooperation Society. 2020;21(8):107–114. http://doi.org/10.5762/KAIS.2020.21.8.107Article
- 38. Jung ES. A study on relationship between infection control job stress, self-efficacy, and professional self-concept of emergency room nurses. [master’s thesis]. [Busan]: Busan Catholic University; 2021. 53 p.
- 39. Choi EH, Byun HS, Kim EH, Keum HS. The effect of a simulation-based integrated clinical practice program on problem-solving competence, critical thinking and clinical competence among nursing students. Crisisonomy. 2016;12(6):125–141. http://doi.org/10.14251/crisisonomy.2016.12.6.125Article
- 40. Yoo EY. Analysis of nursing students' educational needs about Corona19 infection control. Journal of Digital Convergence. 2020;18(12):335–341. http://doi.org/10.14400/JDC.2020.18.12.335Article
- 41. Ji EJ, Seo HE. Effects of simulation based education using standardized patient for contact precaution infection control for nursing students. Journal of Convergence for Information Technology. 2020;10(11):87–97. https://doi.org/10.22156/CS4SMB.2020.10.11.087Article
References
Figure & Data
References
Citations


 KACHN
KACHN
 PubReader
PubReader ePub Link
ePub Link Cite
Cite