Articles
- Page Path
- HOME > Res Community Public Health Nurs > Volume 34(4); 2023 > Article
-
Original Article
- A Multi-component Living Lab on Health Engagement for Advancing Self-care Agency among Migrant Workers in South Korea: A mixed methods study
-
Youlim Kim1
 , Hyeonkyeong Lee2
, Hyeonkyeong Lee2 , Sookyung Kim3
, Sookyung Kim3 , Junghee Kim4
, Junghee Kim4
-
Research in Community and Public Health Nursing 2023;34(4):281-293.
DOI: https://doi.org/10.12799/rcphn.2023.00199
Published online: December 29, 2023
1Assistant Professor, College of Nursing, Kosin University, Busan, Korea
2Professor, College of Nursing, Yonsei University, Seoul, Korea
3Assistant Professor, School of Nursing, Soonchunhyang University, Cheonan, Korea
4Assistant Professor, Wonju College of Nursing, Yonsei University, Wonju, Korea
- Corresponding author: Hyeonkyeong Lee Mo-Im Kim Nursing Research institute, College of Nursing, Yonsei University, Seoul, 50-1 Yonsei-ro, Seodaemun-gu, Seoul, 03722, South Korea Phone: 82-2-2228-3373, Fax: 82-2-392-5440, Email: hlee39@yuhs.ac
Copyright © 2023 Korean Academy of Community Health Nursing
This is an Open Access article distributed under the terms of the Creative Commons Attribution NoDerivs License. (http://creativecommons.org/licenses/by-nd/4.0) which allows readers to disseminate and reuse the article, as well as share and reuse the scientific material. It does not permit the creation of derivative works without specific permission.
- 1,054 Views
- 28 Download
Abstract
-
Purpose
- Migrant workers battle to access health services and adapt to a new culture. Self-care agency can be essential for health self-management. This study examines the effects of a health engagement program to improve self-care agency using a living lab approach among migrant workers living in South Korea.
-
Methods
- This study used a mixed-methods design, including a non-equivalent pre-post-test control group and three focus group interviews. Participants included 42 migrant workers from nine countries recruited via flyers, posters, and internet bulletins posted by a migrant community organization. During the 12 weeks, only the intervention group participants received four workshops addressing healthy physical activity, healthy dietary habits, effective cultural adaptation, stress management, and two outdoor cultural activities. They also participated in focus group interviews after the second, third, and fourth group activities and discussed the benefits of healthy behaviors and specific ways to implement them in real life.
-
Results
- Participants in the intervention group showed an increase in self-care agency, health literacy, and acculturation after the 12-week intervention. Themes were derived based on the lessons from living lab activities, barriers to health behavior practices, and methods to overcome these.
-
Conclusion
- This study demonstrated that multi-component intervention using a living lab effectively increased migrants’ participation in health promotion activities by strengthening health in their self-care agency. The qualitative and living lab approach effectively obtained comprehensive results on strategies to enhance healthy behavior engagement.
- International migration is a worldwide phenomenon, and the various health issues of migrants have become a significant public health concern [1]. Many studies have reported healthcare access for inequalities between migrants and non-migrants [2]. Specifically, limitations in the mental health services usage, language and communication barriers, limitations in primary health care services, and discrimination was prominent. Migrant workers face a significant risk of deteriorating physical and mental health from high levels of physical work, unstable legal status, language barriers, discrimination and culture difference [2]. A study on healthcare behaviors and primary care among migrants found that approximately 30% of respondents reported problems with their self-care activities, such as prescribed medication intake, regular exercise, and monitoring health [3].
- Self-care agency is defined as the complex acquired ability engaging in self-care for maintaining and promoting well-being [4]. Individuals determine their well-being through health-seeking behaviors that involve preventing diseases, care for family, access to and health services [5]. However, in the case of migrant workers, the essential behaviors are limited due to acculturation, which is a multidimensional cultural and psychological change process that results from a contact between two or more different cultures and groups [6]. Consequently, migrant workers with low level of acculturation are likely to have poor health outcomes such as low sleep quality and self-rated health [7]. Considering the vulnerability of migrant workers to cultural adaptation and its expected negative health outcomes, cultivating self-care agency seems to be utmost.
- Social support is another key factor that reduces acculturative stress, depression, perceived discrimination and increase psychological well-being among migrants [8,9]. Furthermore, social support that arises from active participation in host community activities is known to promote a sense of community [10], which facilitates cultural adaptation among migrants [10]. Compared to native ethnic population, low health literacy of migrant workers greatly increased the risk of physical and mental health issues [11] as limiting to understanding, evaluation, and application of health information for health care-related decision-making, disease prevention, and health promotion.
- To our knowledge, intervention programs for migrant workers were primarily focused on workplace safety education, health promotion such as walking and stretching exercises, or disease prevention such as malaria and sexually transmitted infections [12], and are targeted to improve on psychosocial outcomes [13]. To promote engagement in healthy behaviors for migrants, it is essential to gain migrants’ perspectives on self-management. Therefore, in-depth research is needed to emphasize the migrants' health perspective and barriers to healthcare access and increase their self-efficacy toward health management. To encourage migrant workers to engage in health promoting behaviors, it is vital to make them understand its relevance to their lives and empower them to gain control over their environment. The living lab approach is an innovative way of identifying engagement strategies by brainstorming with participants [14]. Living lab is a user-centered environment where users and producers jointly investigate solutions in real-life settings [15]. Especially, it was reported that living lab approaches are more appropriate used to investigate health problems in vulnerable groups [15]. It is also necessary to investigate how migrant workers engage in health promotion behavior. Mixed-methods research practices combine quantitative and qualitative evaluation approaches to understand better research outcomes than when individually used, making it apt to explore living lab interventions effects that co-create interactions in multiple stakeholders and an in-depth understanding of the intervention effects by exploring the participants’ lived experiences [16].
- Health engagement is people's willingness and ability to actively participate in their health and navigate health care services [17], which includes confidence to autonomously manage their health and health literacy [18]. This study aimed to examine the effects of a multi-component health engagement program to improve self-care agency using a living lab approach among migrant workers. Using a mixed-method study design, we applied six principles (multi-method approach, users’ engagement, multi-stakeholder participants, real-life settings, co-creation, and innovation activity) of a living lab [15] to provide intervention for migrant workers and evaluated its effects.
Introduction
- 1. Study design
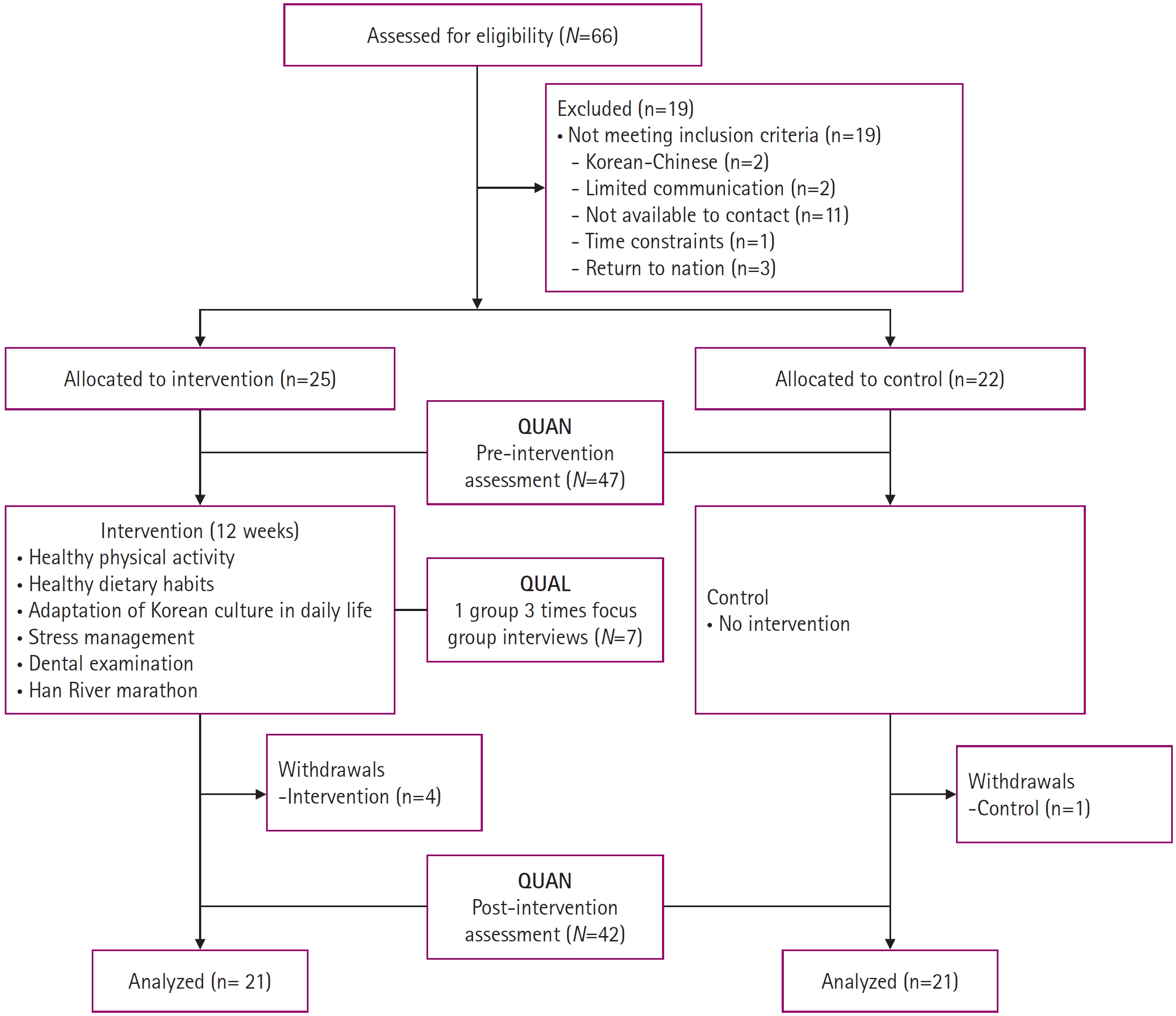
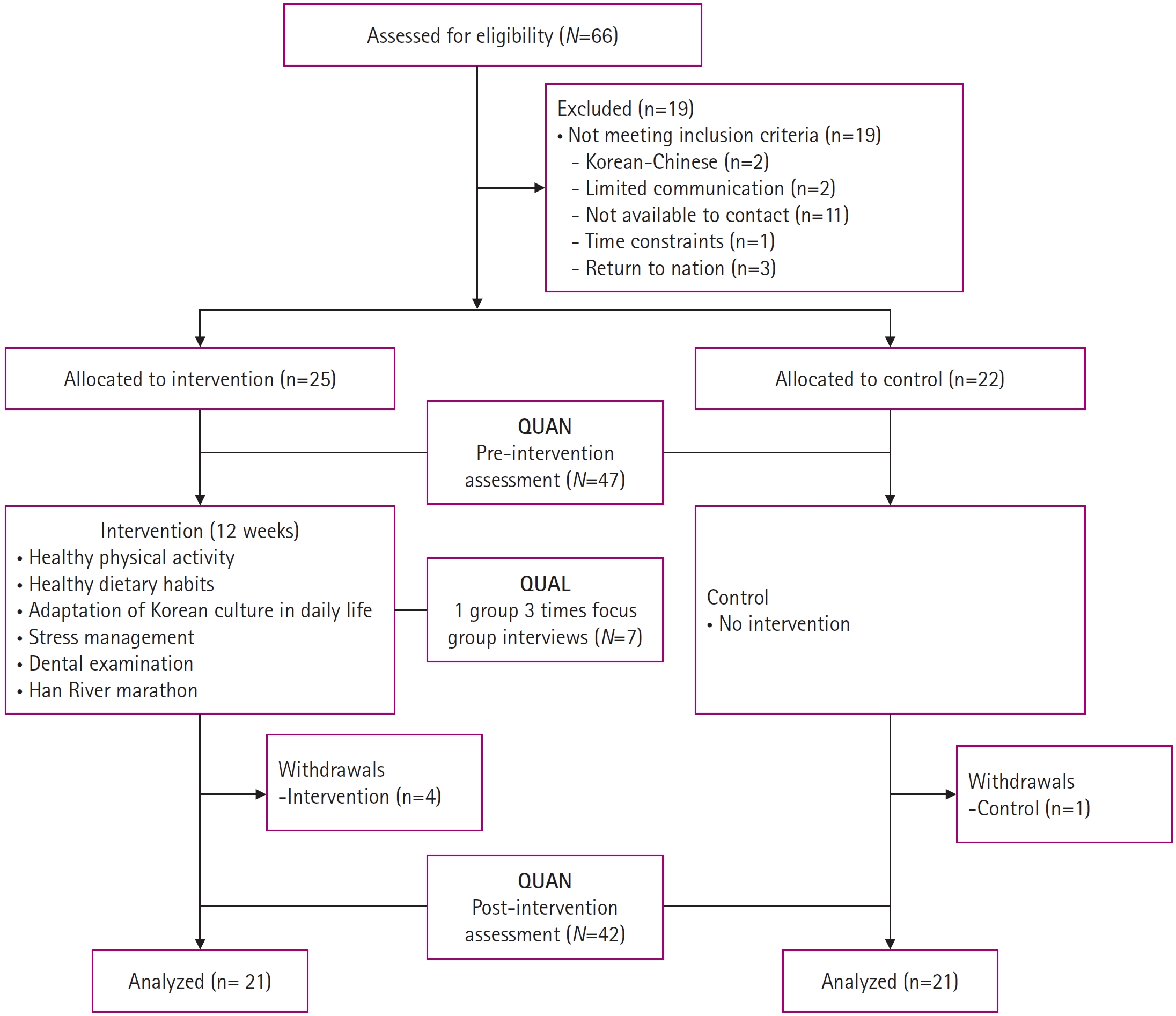
- This study evaluated the effect of a health engagement program for migrant workers using a concurrently embedded mixed-method design combining quantitative (a quasi-experimental research) and qualitative (focus group interviews) research (Figure 1).
- 2. Study sample
- Participants were recruited through invitations on flyers, posters, and internet bulletins of social welfare institutes for migrant workers. The inclusion criteria were migrant workers who were legally employed adults under 40 years of age working full-time, with intermediate-level Korean or Level 3 or higher qualifications in the Test of Proficiency in Korean (TOPIK) and possess a smartphone and the ability to use mobile applications. TOPIK Level 3 is equivalent to intermediate-level Korean language proficiency, ensuring the ability to perform essential language functions necessary for using various public facilities and maintaining social relations without any difficulty for a fully functioning daily life. Illegal migrants and those who had participated in other health promotion programs in the preceding three months were excluded. We initially recruited 66 migrant workers for study participation; however, 19 did not meet the inclusion criteria, and 5 dropped out during the intervention. According to the recruitment order, we assigned them to the intervention (N=25) or control groups (N=22). Finally, data from 42 workers were analyzed, excluding 5 workers who dropped out during the 12-week intervention period (Intervention group: N=21, Control group: N=21). The number of adequate samples required for data analysis was verified by the post hoc test for Wilcoxon-Mann-Whitney test analysis using the G*Power 3.1.9.2 software. The study’s primary outcome, the effect size of the self-care agency, was 1.11, and the significance level was .05, with 21 people in each group; as a result of testing, the statistical power was 92.8%, indicating that the sample size was appropriate.
- 3. Intervention
- This intervention was developed to increase self-care agency in health-promoting lifestyles among migrant workers by refocusing health engagement from the workplace to the individual and strengthening health literacy and health behavior (Table 1). Based on the practical guidelines of the living lab approach [14], which suggested ideas for migrant workers' program participation, this study included multi-component strategies such as health community activities and cultural community activities that the participants could realistically practice and benefit from health. According to a literature review related to self-care [19], some studies applied multi-component interventions to promote self-care and healthy behaviors. Defining a multi-component intervention as an intervention that includes at least two components and settings [20,21] ,this study consisted of health community activities composed of four sessions and cultural community activities including two outdoor activities. To increase the participation of migrant workers in health engagement program, participants freely shared thoughts and opinions about health topics of interest and cultural adaptation activities during orientation. We consisted of the health engagement program based on participants' opinions confirmed during the orientation and data [22] on the health status of migrant workers who reported musculoskeletal injuries, cultural barriers, negative mental health, and so on. During the 12-week intervention period, a total of six sessions, consisting of four health community activities (healthy physical activity, healthy dietary habits, acculturation, and stress management) in the form of workshops involving discussion and practice and two cultural community activities (university tour and dental check-up and marathon participation in a community sports event) in the form of outdoor activities, using community resources were organized. In particular, In particular, to increase the accessibility of intervention participation for hard-to-reach groups, this program was conducted with the cooperation of the Korea Foreign Worker Support Center, which is mainly used by participants.
- All sessions were based on living lab principles, which encouraged participants to solve their health concerns independently. To ensure that participants recognized that the process of participating in the intervention was related to real-life and health in Korea, they discussed their thoughts and how they could apply them to their lives after each session. The first session on “Healthy physical activities” comprised stretching and muscle exercises for migrant workers. The participants learned stretching and muscle exercise movements under the coaching of exercise prescription experts, followed by a discussion about exercise benefits and specific ways to implement them in real life. The second session on “Healthy dietary” comprised information dissemination on a low-sodium diet intake to help cultivate healthy dietary habits. The participants assessed their taste in salt intake with sample foods and were invited to discuss their usual dietary behaviors and healthy dietary practices. Additionally, participants were asked to consult the Ministry of Food and Drug Safety website to find restaurants serving low sodium meals in their neighborhood. The third group activity session on ‘Access to community resources’ aimed to stimulate participants' interest in Korean cultural events and enhance access to community resources by introducing 80 community programs to enable early adaptation and migrant workers’ assimilation into Korean society. Lastly, the participants were introduced to stress management techniques based on a better understanding of their personalities and others using DISC [23], a test tool used for understanding propensity and classifying behavior into four personality types (i.e., Dominant, Influencer, Steady, and Conscientious) to improve communication methods with peers of different personality types. At the session end, participants could identify and understand their personality type and that of others; how migrant workers can communicate better to establish good interpersonal relationships with others was also discussed.
- The contents and location of the cultural activities were decided based on participants’ preferences and previous studies that reported a positive correlation between migrants' participation in cultural activities in the host country and life satisfaction [24,25]. First, based on the study [26] that a higher level of acculturation has a positive effect on health promotion behavior, this study collected opinions from young participants around the age of 30 and conducted a campus tour of a university located in a major tourist attraction in Seoul. The researchers informed them about its history and culture. Additionally, during the tour, they participated in the university hospital's free dental care program and received education on the importance of regular dental care, which motivated them to engage in healthy behaviors. Second, a marathon along the Han River was organized; by combined participation in the five-kilometer marathon, participants and researchers could appreciate the benefits of community resources to organize physical activities and cultural events.
- 4. Study Measures
- The health promotion lifestyle profile was developed by Walker et al. [27] and initially comprised 26 items, but was later shortened [28]. This is a four-point Likert scale (1=never, and 4=routinely), with higher total scores representing better lifestyle conditions for improving health. Cronbach’s α was .70 in this study.
- The health literacy scale was developed by An and Yang [29] to measure the ability of migrant married women to read, write, understand, and use health information. The questionnaire comprises ten items on a five-point Likert scale (0=strongly disagree, and 4=strongly agree). The mean level of health literacy in migrant workers and married women (original study cohort) with intermediate-level Korean was found to be similar. Cronbach’s α was .71 in this study.
- Self-care agency was measured using the Appraisal of Self-Care Agency Scale-Revised (ASAS-R) revised by Sousa et al. [30] and translated into Korean by Kim [31]. The questionnaire comprised 15 items that required responses on a five-point Likert scale (1=strongly disagree, and 5=strongly agree). Scores for self-care agency were directly proportional to the total score. Cronbach’s α was .70 in this study.
- Sense of community was measured using the Korean version of the Brief Sense of Community Scale (BSCS), which was based on the scale developed by Peterson et al. [32] and modified [33]. The scale includes eight items, which had to be rated on the five-point Likert scale (1=strongly disagree, and 5=strongly agree). Some of the BSCS items were changed for the study’s purposes, such as 'peer or friend' to 'neighborhood' and 'peer group' to 'neighbor'. The sense of community score was directly proportional to the total score. Cronbach’s α was .87 in this study.
- Social support was measured using a scale developed [34] and reconstructed [35]. This scale includes 12 items: there were four questions each on support from the family, support from meaningful others, and support from friends. Each response was measured on a five-point Likert scale (1=strongly disagree, and 5=strongly agree). Scores for social support were directly proportional to the total score. Cronbach’s α was .88 in this study.
- Acculturation was measured using a modified and translated Korean questionnaire [36] based on Barry’s East Asian Acculturation Measurement [37]. This scale includes ten items measured on a five-point Likert scale (1=strongly disagree, and 5=strongly agree). The acculturation level was directly proportional to the total score. Cronbach’s α was .72 in this study.
- Focus group interviews were conducted to freely discuss individual experiences, perceptions, and knowledge related to the intervention through active interaction with participants [38]. It included an opening question, an introductory question, a transitional question, key questions, and a final question. Key questions were: “What are the useful conjectures found in this today's health community activity?” “What are the barriers to engaging in healthy behavior in your daily life?” and “How can we overcome barriers and to engage in healthy behavior?”
- 5. Data collection
- This study was conducted from June-September 2019. Researchers trained in ethics explained the study purpose, method, and the process to participants before data collection.
- All participants participated in two surveys: pre-test and post-test. Quantitative data were collected using self-reported questionnaires. Participants who did not understand the questionnaire were provided explanations in person by trained research assistants. Qualitative data were collected on aspects not measured by the survey to supplement the questionnaire results. Due to cooperation in the interview schedule and additional ethical deliberation by the Institutional Review Board, focus group interviews were conducted on the topic with an average of 7 migrant workers only in the 2nd, 3rd, and 4th out of the 4 health community activities. Interviews were conducted in three 40-minute rounds by doctoral students trained in qualitative research methodology. Since migrant workers have slower speech delivery in Korean, interview data were not recorded but transcribed on the spot.
- 6. Data analysis
- Quantitative data were analyzed using SPSS Statistics 25.0 (IBM Corp, Armonk, NY, USA). All continuous variables were described as mean ± standard deviation and categorical variables as frequency. Kolmogorov-Smirnov or Shapiro-Wilk normality verification was conducted, and finally, a non-parametric statistical analysis was selected. Group differences were analyzed using the independent t-test, Mann-Whitney’s U-test, and the Chi-squared test or Fisher’s exact test. The pre-and post-intervention scores of variables were compared and analyzed using Wilcoxon’s signed-rank test. The comparison between the two groups for the mean difference of variables pre-and post-intervention was analyzed using Mann-Whitney's U-test. For the effect size of the study intervention, Cohen's d was calculated due to similar sample sizes among the two groups (https://www.socscistatistics.com/effectsize/default3.aspx). Cohen’s d value was interpreted as the effect size of.20 as a ‘small,'.50 as a 'medium,' and.80 as a 'large.' A p-value <.05 indicates statistical significance.
- Qualitative data were analyzed using qualitative content analysis (QCA); this is based on the context wherein the content was created to derive meaningful interpretations of the themes identified by a systematic reduction of the content [39]. The two researchers read and verified interview transcripts to study migrants’ health engagement experience and willingness to participate in the health behavior program. Meaningful data from the transcripts were extracted, compared, contrasted, and classified, and the main concepts and themes were derived. Additional themes were made to check the validity of the analytical methods used, and the results were further reviewed by one nursing professor with qualitative research experience. The themes that emerged from the analysis were finally agreed upon after discussion between the researchers.
- 7. Ethical Consideration
- Ethical approval was obtained from the Institutional Review Board of the Yonsei University, Seoul, Korea (IRB No.Y-2019-0019). This study was performed following the principles of the Declaration of Helsinki and written informed consent was obtained from study participants.
Methods
3.1. Multi-component intervention for health engagement
3.2. Health community activities
3.3. Cultural community activities
4.1. Health promotion lifestyle
4.2. Health literacy
4.3. Self-care agency
4.4. Sense of Community
4.5. Social support
4.6. Acculturation
4.7. Focus group interviews
- 1. Participants
- Table 2 gives the general characteristics of the participants. The intervention group's mean age and controls were 29.52±3.71 years and 30.67±4.88 years, respectively (p=.363). Participants’ sex had a higher proportion of males in both groups (p=.513). Both groups had a high percentage of participants from countries in the WHO Western Pacific Region (i.e., Cambodia, Mongolia, and Vietnam). The mean duration of their stay in Korea was 59.57±39.49 months in the intervention group and 57.86±37.13 months in the control group (p=.950). The mean number of months worked at the current job was 43.14±23.95 in the intervention group and 37.95±25.35 in the control group (p=.339). The mean time spent working per day was 8.95±1.99 hours in the intervention group and 9.12±1.45 hours in the control group (p=.629). The number of graduates with more than a high school education was 18 (85.7%) in the intervention group and 21 (100.0%) in the control group (p=.072). Regarding the type of job, skilled labor accounted for the largest proportion in both groups. Most participants in both groups were unmarried. The number of participants who smoked was one (4.8%) in the intervention group and two (9.6%) in the control group p=.737. Regarding alcohol intake frequency, the number of participants who consumed less than two glasses per month formed the largest proportion in both groups. There was no statistically significant difference in general characteristics between the intervention and control groups (Table 2).
- 2. Comparison of changes between groups
- Table 3 shows the mean scores for health promotion lifestyle, self-care agency, health literacy, social support, sense of community, and acculturation from baseline to eek 12 in both groups. Self-care agency scores at week 12 compared to baseline significantly increased in the intervention group than in the control group (U= 82.50, p<.001). Compared to the control group, health literacy and acculturation scores over the 12 weeks were significantly increased in the intervention group (U= 91.50, p<.001; U= 119.00, p=.010, respectively). However, changes in health promotion lifestyles, social support, and sense of community scores in the two groups were not significant. In the control group, the level of sense of community at week 12 significantly increased compared to baseline (Z= 2.79, p=.005). The largest effect size was for self-care agency (Cohen’s d= 1.11), with the smallest effect size for social support (Cohen’s d= 0.05).
- 3. Qualitative content analysis of the health engagement intervention
- Various themes were derived based on responses to key questions used in the three focus group discussions with participants in the intervention group (Supplementary material 1), and the topics included a healthy diet, acculturation, and stress management. For each activity, themes were derived based on the lessons learned from living lab activities, barriers to health behavior practices, and methods to overcome these.
- Participants in the health community activities shared what they felt the useful things while participating in each activity. Those who participated in a health community activity on healthy diets said they learned how to estimate their sodium intake using the sodium preference assessment test and had understood the negative health effects of excessive sodium intake. The following themes emerged from this activity: ‘Recognition of the individuals’ salty taste preference,’ ‘Identification of health risks due to dietary imbalances,’ and ‘Necessity to check the nutrition information for families’ health.’
- Those who participated in a health community activity on acculturation found instructions on Korean culture and the use of community resources such as parks as novel experiences. They said this information was necessary for foreigners to adapt. They expressed their acceptance of Korean life and culture. The theme derived from this activity was ‘acceptance and assimilation with Korean culture.’
- Those who participated in a health community activity on stress management said their knowledge of personality types identified through personality tests would help them seek jobs suitable for them. They discussed the need to understand other people's personalities to maintain good interpersonal relationships. The following themes emerged: ‘Understanding of one’s personality’ and ‘Realizing to respect others’ personality.’
- Participants in the health community activities shared what they felt barriers to engagement for healthy behavior in their lives. Barriers to health behavior and acculturation were identified in the categories of intrapersonal, interpersonal, and environmental factors.
- Those who participated in a health community activity on healthy diets said no previous awareness of the importance of nutritional information, and those who lived alone mostly avoided cooking by frequently eating out or ordering food. They also said that poor eating habits formed in their childhood interfered with healthy eating practices in adulthood. The themes that emerged from this activity were ‘Lack of education and awareness of nutrition information,’ ‘Korean culture where people eat out and order in,’ ‘and Unhealthy eating habits.’
- Those who participated in a health community activity on acculturation said the Han River Marathon was their first experience participating in festivals or community events in Korea. Participants showed interest in Korean cultural life and using various community resources but said that access to these was difficult due to a lack of information. Participants used the internet to find information on Korean culture but expressed difficulty with search methods and using tools like the Internet homepage. Based on these, ‘Lack of accessibility to community resource information’ and ‘Difficulty in acculturation due to lack of search ability’ were identified as barriers to the cultural adaptation of migrants.
- Those who participated in a health community activity on stress management expressed they experienced stress due to conflicts with differing personalities, especially when they would force others to follow their perspective. The theme of ‘Lack of respect for other people's personality’ was identified.
- Participants in the health community activities shared what they shared ways to overcome barriers and engage in healthy behaviors in daily life.
- Those who participated in a health community activity on healthy diets said it was important to prepare healthy foods to ensure the health of their families and children. Participants also discussed the importance of improving Korean language skills to read about and prepare healthy food and informing others of their preference for healthy meals. ‘Willingness to cook healthy meals,’ ‘Improving literacy for healthy eating,’ and ‘Changing behavior for healthy eating’ were identified as themes.
- Participants in an acculturation activity agreed that Korean festivals and other cultural events with one another increased their acculturation. Access to Korean cultural life could be increased by using high-powered social networking services such as Facebook. ‘Acculturation to enjoy with participants’ and ‘Using various resources on Korean cultural life’ were identified as themes.
- Those who participated in a health community activity on stress management showed a willingness to overcome personal shortcomings guided by their personality test results. They also expressed the need to think positively and have greater self-confidence to reduce individual stress in a new and unfamiliar environment. Other participants suggested that emotional support through dialogue and humor could help face difficult situations. ‘Understanding of one’s personality and willingness to change attitudes,’ ‘Having a positive mindset and confidence,’ ‘Having an attitude of understanding others,’ and ‘Providing social support to others’ were identified as themes.
Results
1) Awareness of health and acculturation-related information
2) The level of barriers to health behavior and acculturation
3) Personal efforts and social support for healthy behavior and acculturation
- 1. Principal findings
- This study aimed to examine the effects of a multi-components living lab on health engagement among migrant workers. In the intervention group, levels of self-care agency, health literacy, and acculturation at week 12 were significantly increased than in the control group, indicating that the health engagement intervention had been effective. Although migrant workers play a critical role in the labor market as human resources, a significant proportion of migrant workers in South Korea were negatively aware of their self-rated health [40]. Despite the health disparities between migrant and native workers, to our knowledge, no studies on interventions to increase self-care agency for health promotion have been published. Thus, it is worthwhile to show evidence from this study for enhancing health promotion lifestyles of migrant workers.
- Various experimental studies were conducted on migrant workers, including interventions for improving hand-washing skills [41], an educational program on reproductive health [42], culturally tailored HIV risk reduction program [43], peer-facilitated health and safety awareness training [44] and walking exercises for mental health and acculturation [45]. Most of the experimental studies conducted on migrant workers in South Korea were exercise interventions targeting middle-aged Korean-Chinese female workers [46]. Similar to our study, a study providing a multi-component intervention to migrant workers from multi-ethnic backgrounds included language classes and job training courses and reported improved communication with superiors and social support as a result [47]. In South Korea, intervention studies targeting migrant workers were rare, but this study may have significance as an experimental study in that it attempted to improve the targets’ self-care agency by applying multi-component intervention and living lab.
- As a result of qualitative research, it was reported that factors that become barriers to self-care for health behavior include lack of education and awareness, low accessibility to resource information, and difficulties in acculturation due to lack of searching ability. These results were similar to the results of 'lack of knowledge and skills' and 'lack of support' confirmed in a study investigating barriers to exercise performance among migrant workers in South Korea [48]. This evidence based on the results of the participants' interviews provides the importance of strategies such as identifying the barriers perceived by migrant workers, improving health literacy, providing resources for diverse acculturation, and encouraging cultural activities with groups to improve migrant workers' self-care agency in the future. Health interventions for migrant workers with limited access to health information and services at work must be designed in collaboration with workplaces and community resources to ensure a supportive environment for safe and healthy work.
- The living lab is an open network of people, which can encourage rapid and dynamic community participation. Living lab principles were applied as intervention strategies in this study to encourage in-depth exploration and active participation of migrant workers in health behavior engagement. Hard-to-reach (HTR) populations such as migrants and disabled people reported to be alienated from regular communication channels for various reasons [14] are typically hesitant about participating in health programs [49]. This study designed interventions using a guide that includes strategies and advice to help migrant workers easily access and continue to participate in health issues as an HTR population. Thus, we could persuade migrant workers that participation in user-driven programs is beneficial. Ultimately, participation was intended to help increase self-care agency in migrant workers and acculturation in Korea. In another study centered on marginalized groups in the community, the living lab method helped increase health and media literacy and resolved health disparities through cooperation with various stakeholders [50].
- Combining mixed methods with action research methods such as living lab and intervention assessment yielded credible and valid conclusions about the intervention results and maximized the study potential [51]. Using solely quantitative research methods would have limited the identification of the various experiences and attitudes of the health promotion activities among migrant workers. Focus group interviews were used to discuss health issues; these discussions also provided co-learning opportunities and enabled multi-dimensional dynamics such as behavior motivation and results. The results of our qualitative research could be used in future studies to help plan interventions for health-promoting behaviors.
- Our study results showed that the multi-component living lab increased access to community information and resources, such as social and health services in the host country and increased cultural adaptation. From a socioecological viewpoint, creating a supportive social environment, with opportunities for cultural activities and recreation and a comfortable physical environment, would promote migrants’ acculturation and health and ensure their better control over health [52]. Participating in the host country’s cultural activities, such as sporting or social events [25,47], is also a positive predictor of well-being as migrants may feel a greater sense of assimilation with the host society.
- Global migration has expanded widely around world but reducing the health and safety gap for migrants in the workplace remains a challenge. Existing studies have uncovered various risk factors such as poor working conditions and acculturative stress for migrant workers, but sustainable interventions to improve self-management skills have been limited. Importantly, this study adds to the current knowledge that the living lab methodology was useful for the program development stage to identify their needs and to co-create program contents with various stakeholders so that stimulate motivation for program participation and evaluation. The health intervention applying the living lab in this study is meaningful that it showed the results of attempting to integrate the cultural adaptation of migrant workers as well as health issues by linking the host country's participation in cultural activities. Migrants-centered health interventions that focus on the potential of migrants improve health understanding and cultural adaptation than native-centered interventions through problem-oriented approaches [53]. This suggests the need to build partnerships with community organizations in which migrants participate in implementing migrant health programs. Finally, it is suggested to identify the effectiveness of the program and how socially vulnerable migrant workers can be best supported through longitudinal studies.
- This study has tried to comply with living lab principles such as user engagement, multi-methods and co-creation during the intervention process. However, the migrant participants lacked the dynamism to recognize health issues and find solutions about how they could improve everyday actions for a healthy lifestyle. This may be due to language barriers and lack of acculturation, although only participants with intermediate-level Korean were selected. However, the mixed methods helped identify significant results that reflect the participants' unique characteristics. After each intervention activity, the three-group discussion was insufficient for all participants to share their beliefs and health value and commit to the engagement in healthy lifestyle behaviors. Considering these limitations, occupational health professionals and researchers can develop interventions by the ethnic group who speak the same language for a sufficient time period in collaboration with community stakeholders with bilingual and bicultural competency.
Discussion
- This study examined the effects of a 12-week multi-component living lab for migrant workers to promote acculturation and healthy behavior engagement. The intervention group showed statistically significant differences in self-care agency, health literacy, and acculturation than in the control group. Living lab approach combined with mixed-method research were useful for researchers to identify effective strategies for encouraging migrant workers to make self-health decisions and to engage in self-management.
Conclusion
SUPPLEMENTARY MATERIALS
Supplementary material 1.
-
Conflict of interest
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and publication of this article.
-
Funding
This work was supported by the National Research Foundation of Korea (NRF) grant funded by the Korea government (NRF-2017R1A2B4008671, 2020R11A2069894) and the Brain Korea 21 FOUR Project, College of Nursing, Yonsei University by the NRF of Korea.
-
Authors’ contributions
Youlim Kim contributed to conceptualization, formal analysis, methodology, investigation, visualization, and writing-original draft, review & editing. Hyeonkyeong Lee contributed to conceptualization, funding acquisition, methodology, writing-original draft, review & editing, and supervision. Sookyung Kim contributed to formal analysis and writing-review & editing. Junghee Kim contributed to formal analysis and writing-review & editing.
-
Data availability
The data that support the findings cannot be made publicly available as data sharing is not covered by the informed consent.
-
Trial Registration
The study protocol was registered in the World Health Organization International Clinical Trials Portal (KCT0006584; https://trialsearch.who.int/Trial2.aspx?TrialID=KCT0006584, 2021-09-16).
NOTES
Acknowledgments
- 1. Global Migration Indicatiors. Global Migration Data Analysis Centre. International Organization for Migration [Internet]. Berlin: International Oragnization For Migrantion. 2018 [cited 2020 May 18]. Available from: https://publications.iom.int/system/files/pdf/global_migration_indicators_2018.pdf
- 2. Adhikary P, Sheppard ZA, Keen S, Teijlingen Ev. Health and well-being of Nepalese migrant workers abroad. International Journal of Migration, Health and Social Care. 2018;14(1):96–105. https://doi.org/10.1108/IJMHSC-12-2015-0052Article
- 3. Moreno G, Morales LS, Batts F, Noguera C, Isiordia M, Mangione CM. Migration, health care behaviors, and primary care for rural latinos with diabetes. Journal of Immigrant and Minority Health. 2016;18(5):1247–1252. https://doi.org/10.1007/s10903-015-0254-5ArticlePubMedPMC
- 4. Orem DE, Taylor S, Renpenning K. Nursing Concept of Practice. 6th ed. ST Louis: Mosby A Harcout Health Scienc Company; 2001. 542 p.
- 5. Narasimhan M, Kapila M. Implications of self-care for health service provision. Bulletin of the World Health Organization. 2019;97(2):76. http://doi.org/10.2471/BLT.18.228890ArticlePubMedPMC
- 6. Berry JW. Acculturation: Living successfully in two cultures. International Journal of Intercultural Relations. 2005;29(6):697–712. https://doi.org/10.1016/j.ijintrel.2005.07.013Article
- 7. Gonzalez-Guarda RM, Stafford AM, Nagy GA, Befus DR, Conklin JL. A systematic review of physical health consequences and acculturation stress among Latinx individuals in the United States. Biological Research for Nursing. 2021;23(3):362–374. https://doi.org/10.1177/1099800420968889ArticlePubMedPMC
- 8. Hashemi N, Marzban M, Sebar B, Harris N. Perceived discrimination and subjective well-being among Middle Eastern migrants in Australia: The moderating role of perceived social support. International Journal of Social Psychiatry. 2021;67(2):110–119. https://doi.org/10.1177/0020764020940740ArticlePubMed
- 9. Fang CY, Handorf EA, Rao AD, Siu PT, Tseng M. Acculturative stress and depressive symptoms among chinese immigrants: the role of gender and social support. Journal of Racial and Ethnic Health Disparities. 2021;8(5):1130–1138. https://doi.org/10.1007/s40615-020-00869-6ArticlePubMedPMC
- 10. Bostean G, Gillespie BJ. Acculturation, acculturative stressors, and family relationships among Latina/o immigrants. Cultural Diversity and Ethnic Minority Psychology. 2018;24(1):126–138. https://doi.org/10.1037/cdp0000169ArticlePubMed
- 11. Lee JM, Lee E. Factors influencing level of health literacy of migrant workers in Korea. Journal of Korean Academy of Fundamentals of Nursing. 2013;20(3):269–277. https://doi.org/10.7739/jkafn.2013.20.3.269Article
- 12. Mucci N, Traversini V, Giorgi G, Garzaro G, Fiz-Perez J, Campagna M, et al. Migrant workers and physical health: An umbrella review. Sustainability. 2019;11(1):232. https://doi.org/10.3390/su11010232Article
- 13. Kim JH, Park SJ, Lee JA. Effects of intervention for health promotion of foreign workers: A systematic review. Journal of the Korea Convergence Society. 2018;9(9):407–420. https://doi.org/10.15207/JKCS.2018.9.9.407Article
- 14. Pappers J, Keserü I, Macharis C. Report on the methodology for the inclusion of hard-to-reach groups [Internet]. European Union: Urban Europe. 2018 [cited 2020 May 18]. Available from: http://looperproject.eu/wp-content/uploads/2018/10/LOOPER_D3.2_Hard_to_Reach_Groups_FINAL.pdf
- 15. Kim J, Kim YL, Jang H, Cho M, Lee M, Kim J, et al. Living labs for health: An integrative literature review. European Journal of Public Health. 2020;30(1):55–63. https://doi.org/10.1093/eurpub/ckz105ArticlePubMed
- 16. Creswell JW, Clark VLP. Designing and conducting mixed methods research: Sage publications; 2017. 488 p.
- 17. Friis K, Lasgaard M, Osborne RH, Maindal HT. Gaps in understanding health and engagement with healthcare providers across common long-term conditions: A population survey of health literacy in 29 473 Danish citizens. BMJ Open. 2016;6(1):e009627. https://doi.org/10.1136/bmjopen-2015-009627ArticlePubMedPMC
- 18. Smith SG, Curtis LM, Wardle J, von Wagner C, Wolf MS. Skill set or mind set? Associations between health literacy, patient activation and health. PloS one. 2013;8(9):e74373. https://doi.org/10.1371/journal.pone.0074373ArticlePubMedPMC
- 19. Oliveira D, Sousa L, Orrell M. Improving health-promoting self-care in family carers of people with dementia: A review of interventions. Clinical Interventions in Aging. 2019;14:515–523. https://doi.org/10.2147/CIA.S190610ArticlePubMedPMC
- 20. He J, Wang J, Zhong H, Guan C. The effectiveness of multi-component interventions on the positive and negative aspects of well-being among informal caregivers of people with dementia: A systematic review and meta-analysis. International Journal of Environmental Research and Public Health. 2022;19(12):6973. https://doi.org/10.3390/ijerph19126973ArticlePubMedPMC
- 21. Özbe D, Graessel E, Donath C, Pendergrass A. Immediate intervention effects of standardized multicomponent group interventions on people with cognitive impairment: A systematic review. Journal of Alzheimer's Disease. 2019;67(2):653–670. https://doi.org/10.3233/jad-180980Article
- 22. Moyce SC, Schenker M. Migrant workers and their occupational health and safety. Annual Review of Public Health. 2018;39:351–365. https://doi.org/10.1146/annurev-publhealth-040617-013714ArticlePubMed
- 23. Slowikowski MK. Using the DISC behavioral instrument to guide leadership and communication. AORN Journal. 2005;82(5):835–843. https://doi.org/10.1016/S0001-2092(06)60276-7ArticlePubMed
- 24. Gülnar B, Balcı Ş. The relationship between life satisfaction, interpersonal communication and media using among foreign students. International Journal of Multidisciplinary Thought. 2012;2(2):43–54.
- 25. Gunasekara A, Grant S, Rajendran D. Years since migration and wellbeing among Indian and Sri Lankan skilled migrants in Australia: Mediating effects of acculturation. International Journal of Intercultural Relations. 2019;70:42–52. https://doi.org/10.1016/j.ijintrel.2019.02.006Article
- 26. Kim SJ, Yoo IY. Health promotion behavior of Chinese international students in Korea including acculturation factors: A structural equation model. Asian Nursing Research. 2016;10(1):25–31. https://doi.org/10.1016/j.anr.2015.10.008ArticlePubMed
- 27. Walker SN, Sechrist KR, Pender NJ. Health promotion model-instruments to measure health promoting lifestyle: Health-promoting lifestyle profile [HPLP II](Adult version) [Internet]. NE: University of Nebraska Medical Cener. 1995 [cited 2019 Feb 12]. Available from: http://hdl.handle.net/2027.42/85349
- 28. Jeon EY, Choi SR, Han SS. Influencing factors on health-promotion lifestyle of nurses. Journal of East-West Nursing Research. 2007;13(1):40–47.
- 29. An J, Yang SJ. Development of a health literacy assessment scale for Asian immigrant women in South Korea. Journal of Korean Academy of Community Health Nursing. 2015;26(4):330–341. https://doi.org/10.12799/jkachn.2015.26.4.330Article
- 30. Sousa VD, Zauszniewski JA, Bergquist‐Beringer S, Musil CM, Neese JB, Jaber AaF. Reliability, validity and factor structure of the Appraisal of Self‐Care Agency Scale–Revised (ASAS‐R). Journal of Evaluation in Clinical Practice. 2010;16(6):1031–1040. https://doi.org/10.1111/j.1365-2753.2009.01242.xArticlePubMed
- 31. Kim HG. Relationship of self-care agency and educational needs in lung cancer patients with pulmonary resection [master's thesis]. [Seoul]: Yonsei University; 2012. 80 p.
- 32. Peterson NA, Speer PW, McMillan DW. Validation of a brief sense of community scale: Confirmation of the principal theory of sense of community. Journal of Community Psychology. 2008;36(1):61–73. https://doi.org/10.1002/jcop.20217Article
- 33. Oh JH, Kim CW, Ha MH. A study on effect of adolescents’ leisure satisfaction on self-esteem and sense of community: Focused on vocational high school students. International Journal of Tourism and Hospitality Research. 2012;26(2):23–40.
- 34. Zimet GD, Dahlem NW, Zimet SG, Farley GK. The multidimensional scale of perceived social support. Journal of Personality Assessment. 1988;52(1):30–41. https://doi.org/10.1207/s15327752jpa5201_2Article
- 35. Shin JS, Lee YB. The effects of social supports on psychosocial well-being of the unemployed. Korean Jounal of Social Welfare. 1999;37:241–269.
- 36. Jang JY. Influence that marital satisfaction and fostering stress of marriage immigrating women has on the cultural adaptation [master's thesis]. [Seoul]: Chung-Ang University; 2009. 104 p.
- 37. Barry DT. Development of a new scale for measuring acculturation: The East Asian Acculturation Measure (EAAM). Journal of Immigrant Health. 2001;3(4):193–197. https://doi.org/10.1023/A:1012227611547ArticlePubMed
- 38. Krueger RA. 5th ed. Focus groups: A practical guide for applied research. CA: Sage publications; 2014. 280 p.
- 39. Roller MR, Lavrakas PJ. Applied qualitative research design: A total quality framework approach. NY: Guilford Publications; 2015. 398 p.
- 40. Chae DH, Kang KH. Factors associated with the self-rated health of married immigrant women in South Korea. Journal of Korean Public Health Nursing. 2021;35(2):224–238. https://doi.org/10.5932/JKPHN.2021.35.2.224Article
- 41. Yang C, Hu J, Tao M, Li Y, Chai Y, Ning Y, et al. Effectiveness of a multifaceted intervention on improving the hand-washing skills and behaviors of migrant workers in Beijing. Global Health Promotion. 2017;24(3):32–39. https://doi.org/10.1177/1757975915601833ArticlePubMed
- 42. Zhu C, Geng Q, Chen L, Yang H, Jiang W. Impact of an educational programme on reproductive health among young migrant female workers in Shenzhen, China: An intervention study. International Journal of Behavioral Medicine. 2014;21(4):710–718. https://doi.org/10.1007/s12529-014-9401-yArticlePubMed
- 43. Sanchez M, Rojas P, Li T, Ravelo G, Cyrus E, Wang W, et al. Evaluating a culturally tailored HIV risk reduction intervention among Latina immigrants in the farmworker community. World Medical & Health Policy. 2016;8(3):245–262. https://doi.org/10.1177/0890117118807716ArticlePubMedPMC
- 44. Williams Jr Q, Ochsner M, Marshall E, Kimmel L, Martino C. The impact of a peer-led participatory health and safety training program for Latino day laborers in construction. Journal of Safety Research. 2010;41(3):253–261. https://doi.org/10.1016/j.jsr.2010.02.009ArticlePubMed
- 45. Kim Y, Lee YM, Cho M, Lee H. Effect of a pedometer-based, 24-week walking intervention on depression and acculturative stress among migrant women workers. International Journal of Environmental Research and Public Health. 2019;16(22):4385. https://doi.org/10.3390/ijerph16224385ArticlePubMedPMC
- 46. Yang YR, Kim HY. Network analysis for trends in health-related research on immigrant workers living in Korea: During the past 10 years(2010-2019). Korean Public Health Research. 2021;47(1):59–75. https://doi.org/10.22900/kphr.2021.47.1.006Article
- 47. Smith LH, Hviid K, Frydendall KB, Flyvholm MA. Improving the psychosocial work environment at multi-ethnic workplaces: A multi-component intervention strategy in the cleaning industry. International Journal of Environmental Research and Public Health. 2013;10(10):4996–5010. https://doi.org/10.3390/ijerph10104996ArticlePubMedPMC
- 48. Lee H, Wilbur J, Chae D, Lee K, Lee M. Barriers to performing stretching exercises among Korean‐Chinese female migrant workers in Korea. Public Health Nursing. 2015;32(2):112–121. https://doi.org/10.1111/phn.12105ArticlePubMed
- 49. Ellard-Gray A, Jeffrey NK, Choubak M, Crann SE. Finding the hidden participant: Solutions for recruiting hidden, hard-to-reach, and vulnerable populations. International Journal of Qualitative Methods. 2015;14(5):1609406915621420. https://doi.org/10.1177/1609406915621420Article
- 50. Cooke-Jackson A. Chapter 11 - Urban Communities as Locations for Health, Media Literacy and Civic Voice. In: M. Dezuanni, M. Foth, K. Mallan, H. Hughes, editors. Digital Participation through Social Living Labs. England: Chandos Publishing; 2018. p. 207–222.https://doi.org/10.1016/B978-0-08-102059-3.00011-3
- 51. Ivankova N, Wingo N. Applying mixed methods in action research: Methodological potentials and advantages. American Behavioral Scientist. 2018;62(7):978–997. https://doi.org/10.1177/0002764218772673Article
- 52. World Health Organization. Regional Office for Europe. Health 2020: A European policy framework and strategy for the 21st century [Internet]. Copenhagen: World Health Organization. Regional Office for Europe. 2013 [cited 2020 May 18]. Available from: https://apps.who.int/iris/handle/10665/326386
- 53. Pelters P, Lindgren EC, Kostenius C, Lydell M, Hertting K. Health-related integration interventions for migrants by civil society organizations: An integrative review. International Journal of Qualitative Studies on Health and Well-being. 2021;16(1):1927488. https://doi.org/10.1080/17482631.2021.1927488ArticlePubMedPMC
References
Figure & Data
References
Citations


 KACHN
KACHN
 PubReader
PubReader ePub Link
ePub Link Cite
Cite