Articles
- Page Path
- HOME > J Korean Acad Community Health Nurs > Volume 32(4); 2021 > Article
- Original Article Factors Affecting the Quality of Sleep in Young Adults
- Ae Kyung Chang, Kyung Hye Lee, Chong Mi Chang, Jin Yi Choi
-
DOI: https://doi.org/10.12799/jkachn.2021.32.4.497
Published online: December 31, 2021

2Associate Professor, Department of Nursing Science, Suwon Science College, Hwaseong, Korea

3Associate Professor, Department of Nursing, Yong-In Arts & Science University, Yongin, Korea

4Associate Professor, Department of Nursing, Konkuk University, Chungju, Korea

- 1,351 Views
- 78 Download
- 0 Crossref
- 0 Scopus
Abstract
Purpose
The study aimed to identify the effects of sleep hygiene (use of caffeine, alcohol, night eating syndrome, stress, and coping styles), social network, and smartphone-related factors on quality of sleep in young adults.
Methods
This was a descriptive research design. Participants completed a questionnaire on evidence-based variables including caffeine intake, alcohol consumption, social network, night eating syndrome, stress, coping styles, and smartphone-related factors. Stepwise multiple regression was used for data analysis to identify factors that influenced the participants’ quality of sleep. This study included 288 young adults in South Korea.
Results
This study identified the factors affecting quality of sleep in young adults. Their average weekly sleep duration was 6.86 hours with low sleep quality, indicated by a score of 59.34 points (range 17-100). The predictors of sleep quality were sleep mood, sub-items of night eating syndrome, effects of pain over the last four weeks, and social networks, which explained 33% of the variance.
Conclusion
Sleep-induced diseases in young adults could be prevented by identifying sleep mood, pain, and social networks, which is important for health and using them as a basis for intervention.
| J Korean Acad Community Health Nurs. 2021 Dec;32(4):497-505. English. Published online Dec 29, 2021. https://doi.org/10.12799/jkachn.2021.32.4.497 | |
| © 2021 Korean Academy of Community Health Nursing | |
Ae Kyung Chang ,1
Kyung Hye Lee ,1
Kyung Hye Lee ,2
Chong Mi Chang ,2
Chong Mi Chang ,3
and Jin Yi Choi ,3
and Jin Yi Choi 4 4
| |
|
1Associate Professor, College of Nursing Science, Kyung Hee University, Seoul, Korea. | |
|
2Associate Professor, Department of Nursing Science, Suwon Science College, Hwaseong, Korea. | |
|
3Associate Professor, Department of Nursing, Yong-In Arts & Science University, Yongin, Korea. | |
|
4Associate Professor, Department of Nursing, Konkuk University, Chungju, Korea. | |
Corresponding author: Choi, Jin Yi. Department of Nursing, Konkuk University, 268 Chungwon-daero, Chungju 27478, Korea. Tel: +82-43-840-3959, Fax: +82-43-840-3958, | |
| Received July 12, 2021; Revised October 24, 2021; Accepted November 01, 2021. | |
|
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by- | |
|
Abstract
| |
|
Purpose
The study aimed to identify the effects of sleep hygiene (use of caffeine, alcohol, night eating syndrome, stress, and coping styles), social network, and smartphone-related factors on quality of sleep in young adults.
Methods
This was a descriptive research design. Participants completed a questionnaire on evidence-based variables including caffeine intake, alcohol consumption, social network, night eating syndrome, stress, coping styles, and smartphone-related factors. Stepwise multiple regression was used for data analysis to identify factors that influenced the participants’ quality of sleep. This study included 288 young adults in South Korea.
Results
This study identified the factors affecting quality of sleep in young adults. Their average weekly sleep duration was 6.86 hours with low sleep quality, indicated by a score of 59.34 points (range 17-100). The predictors of sleep quality were sleep mood, sub-items of night eating syndrome, effects of pain over the last four weeks, and social networks, which explained 33% of the variance.
Conclusion
Sleep-induced diseases in young adults could be prevented by identifying sleep mood, pain, and social networks, which is important for health and using them as a basis for intervention. |
|
Keywords:
Sleep hygiene; Young adult; Smartphones
|
|
|
INTRODUCTION
|
Sleep is a mechanism for restoring bodily functions and for maintaining energy, health, and essentially a balance between sleep and activity. The amount of sleep recommended for adults is 7~8 hours. If sleep duration is decreased in adults, chances of cardiovascular diseases, stroke, and metabolic syndrome increase, while fasting insulin sensitivity and inflammatory markers might reduce [1, 2]. Lack of sleep in young adults has a negative effect on their attention [3]. Young adults are active in social life and work, hence they are physically active. If their sleep is insufficient, their concentration decreases and problems in physical and mental health management and normal social life may occur [3]. Despite its importance, insufficient sleep is an increasing problem throughout the world.
The average amount of sleep in adults, aged 19 years or older, in Korea is 7.85 hours [4]. This is the lowest among all the member countries of the Organization for Economic Co-operation and Development [4]. Unpleasant changes in sleep, brought about by aging, are not only seen in older adults but also young adults and middle-aged people. The sleep quality of young adults is usually low [5, 6]. Fifty to seventy million adults in the United States have sleep disorders, and 37.9% of adults reported experiencing unexpected sleepiness at least once during the day [7]. Since most research studies on sleep have focused primarily on people in their 40s and above, or older adults, there has been insufficient research on the subject of young adults.
Factors that influence quality of sleep in adults include gender, emotion, an increase in body mass index (BMI) and abdominal circumference, obesity, physical activity, sedentary lifestyle, stress, coping style, drinking, smoking, and pain [8]. Emotions have both, positive and negative effects on quality of sleep. Stress level, which has a negative effect on quality of sleep, is the highest among adults aged 19 to 38 years [8, 9]. Moreover, in some studies, stress coping styles such as hobbies, exercise, and optimistic thinking had a positive effect on quality of sleep; exercise and hobbies, in particular, were effective in improving the subjective quality of sleep among young adults [10, 11]. For young adults, recently, smartphone addiction and binge drinking are the most influential factors of sleep [3, 12, 13, 14, 15], but caffeine consumption is the highest among adults aged 18 to 30 years, and high intake of caffeine also has a negative effect on quality of sleep [16].
Sleep hygiene means having both a bedroom environment and daily routines that promote consistent, uninterrupted sleep. Sleep hygiene includes diet; nicotine, caffeine, and alcohol intake; stress; emotional status and physical activity; and physical factors [8]. Binge drinking and night eating are common dietary factors in young adults [15, 17]. Binge drinking is defined as consuming five or more drinks by men and four or more drinks by women within 2 hours. Rates of binge drinking rate in Korea are over 50.0% for men in their 30s to 50s, and 44.1% for women in their 20s [9]. In other countries, binge drinking is common in college students and young adults [14, 15]. It is closely related to sleep disorders associated with psychological problems [15]. Another factor that is unique to young adults is night eating. Night eating syndrome is more commonly reported among young adults in their 30s and college students, than in older adults [17]. Night eating syndrome causes several health-related problems-including sleep disorders, stress, depression, and obesity-as it is related to the discrepancy between sleep cycles and food intake rhythms.
Korea has the highest penetration rate of smartphones worldwide, and 83.6% of its total population uses smartphones [18]. The number of individuals in potential-risk or high-risk groups for smartphone addiction is 3~4 times higher among those in their 20s and 30s, than in their 60s and older. Women are also more susceptible to smartphone addiction than men. Moreover, these trends are increasing [18]. Although smartphones have many advantages, their excessive use negatively affects sleep and health. Excessive smartphone use among young adults leads to a more sedentary lifestyle, problems and dependence in personal relationships, anxiety, loneliness, depression, and insomnia [5]. In particular, the blue light emitted by smartphones has negative effects on sleep [13, 19].
Another important factor related to sleep is social networks, a multidimensional concept that encompasses the size and components of social relationships; the frequency with which one contacts family, friends, and spouse; the degree to which help is given or received; and the degree of satisfaction with one’s social relationships [20]. Among older adults, emotional support and bonding provided through social networks, reduces the effect of stress-induced depression, while weak social networks lead to high levels of stress and depression, which indirectly have a negative effect on sleep [4]. Social networks for young adults, however, are closely related to addictive behaviors such as drinking and smoking, which also have negative effects on sleep [12].
When the factors affecting sleep were examined, physical health status had a greater effect on sleep in middle-aged and older adults, whereas emotional factors, drinking, work hours, stress and coping styles, and smartphone usage had a greater effect on sleep in young adults with relatively good health status [5, 12, 15]. Additionally, sleep hygiene includes overuse of smartphone and lack of a social network [5, 12, 21]. Physical and emotional aspects such as hormones, pain, and depression usually have negative effects on the sleep of older adults or middle-aged individuals. However, in young adults, the increase in social gatherings, smartphone addiction, and alcohol abuse, delay the start-up time and negatively affect sleep [21, 22]. Therefore, we analyzed to identify the effects of sleep hygiene (caffeine intake, alcohol drinking, night eating syndrome, stress coping styles, sedentary lifestyle), social networks, and smartphone-related factors on the quality of sleep in young adults, to provide basic information for developing interventions for young adults with sleep problems.
|
METHODS
|
1. Design
This study aimed to identify the effects of sleep hygiene (caffeine intake, alcohol drinking, night eating syndrome, stress, and coping styles, sedentary lifestyle), along with the effects of smartphone and social network-related factors, on quality of sleep in young adults. This study used a descriptive research design.
2. Sample
The participants of this study were employed young adults aged between 19 and 39 years. The selection criteria were: adults aged 19 to 39 years who understood the purpose of this study and agreed to participate in it. Meanwhile, the exclusion criteria were: being diagnosed with depression or sleep disorders within the last six months and taking medication. The sample size was calculated as 242, with a significance level of .05, a medium effect size of .15, power of 95.0%, and 25 predictors in linear multiple regression analysis using the G-power 3.1.5 software program (Heinrich Heine University, Dusseldorf, Germany). A self-report questionnaire survey was conducted using the Internet or a mobile phone, and a total of 288 participants completed it except for 2 subjects whose questionnaire was incomplete.
3. Measures
Sleep duration was divided into weekdays and weekends, and the average sleep duration was measured using self-report. The quality of sleep was measured using the Korean version of the Modified Leeds Sleep Evaluation Questionnaire (KMLSEQ) [23]. The KMLSEQ consists of 10 questions in four dimensions related to going to sleep, quality of sleep, waking after sleep, and behavior after waking up. A higher score indicates better quality of sleep. The Cronbach’s α in the study by Kim et al. [23] was 0.95 and 0.84 in this study.
In this study, night eating syndrome was measured using the Korean version of the Night Eating Questionnaire (KNEQ) translated and modified by Kim et al. [24]. This tool consists of four categories: morning anorexia, evening hyperphagia, nocturnal ingestion, and mood/sleep. This tool examines the awareness of night eating for the differential diagnosis between parasomnia and a sleep-related eating disorder. The 14 questions are scored based on a five-point scale in which a higher total score indicates a more severe degree of night-eating syndrome. The Cronbach's α of the tool during development was 0.70, 0.78 during translation [24], and 0.68 in this study.
In this study, social networks were analyzed using the Lubben Social Network Scale-Revised (LSNS-R) which was translated and made available on the web by Hong et al. [25]. It consists of a total of 12 questions including two factors, family and friends, each comprising six questions. The six questions include the number of people with whom a person is in contact, frequency of contact, number of people with whom the person can speak freely, number of people they can ask for help, frequency of advising on important decisions, and frequency of receiving advice regarding important decisions. Each question is scored on a six-point scale, where a higher average score indicates a wider social network. The Cronbach's α of the tool was 0.84 during translation [25] and 0.89 in this study.
Smartphone-related factors in this study included the characteristics and time spent using a smartphone and the degree of overdependence thereon. To evaluate the characteristics of smartphone usage, a tool modified by Lee [26] was used. This tool consists of a total of 22 questions scored on a five-point scale in four subcategories: communication, information, leisure, and convenience. The Cronbach's α of the tool used in the study by Lee [26] was 0.86 and 0.79 in this study. To measure smartphone overdependence, we used a self-diagnostic scale of smartphone addiction for adults [27]. To measure smartphone overdependence, we used a self-diagnostic scale for smartphone addiction for adults, which combined the existing Internet (K-scale) and smartphone (S-scale) scales from 2016 [27]. This tool consists of a total of 10 questions scored on a four-point scale in three subcategories: self-control failure, salience, and serious consequence. A score of 29 points or above is considered high-risk, while 24~28 points fall into the potential-risk group for adults. The Cronbach's α of the tool during development was 0.86 [27] and in 0.89 in this study. Stress coping styles were examined using the Situational Version of Coping Orientation to Problems Experienced (Brief COPE) [28]. This tool consists of 28 questions in four subcategories and was modified in 2015 to include 14 items. Each answer was self-reported based on a four-point Likert scale. A higher score indicates more effort to cope with stress and use coping styles. The Cronbach's α of the tool during development was 0.90 [28] and 0.80 in this study.
We measured the participants' gender, age, occupation, subjective health status, stress level, pain over the last four weeks, BMI, drinking frequency and binge drinking status, smoking, daily caffeine intake (mg/day), and daily sedentary duration. Subjective health status and stress level were measured based on a five-point scale using one question in which a higher score indicates better subjective health status and lower stress levels.
4. Ethical Considerations and Data Collection Procedure
Ethical approval for the study was obtained by the ethics review board of the Suwon Science college (IRB NO.: IRB2-7008167-AB-N-01-202102-HR-001-02). All participants read and understood the purpose of the study, participated voluntarily, and signed an online informed consent form. Data were collected from February 2021 to March 2021. After seeing the announcement on the bulletin board, if anyone interested in contacting us, we sent a link via smartphone SMS or mail. Before starting the online questionnaire, subjects were allowed to start only after reading the consent form and signing online. A self-report questionnaire survey was conducted using the Internet or a mobile phone, and a total of 288 participants completed it.
5. Statistical Analysis
Frequencies and percentages are reported for categorical variables, while mean, and standard deviation (SD) are reported for continuous variables. Differences in quality of sleep and sleeping time by general characteristics were analyzed with analysis of variance (ANOVA) and t-tests. Significant variables in ANOVA were subjected to Scheffe?’s post hoc test. Pearson's correlation coefficient was used to measure the statistical relationships among the variables. Stepwise multiple linear regression was performed to identify factors that influenced the participants' quality of sleep by considering all statistically significant variables as response variables. The significance level was set at 0.05.
|
RESULTS
|
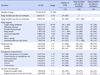
Quality of Sleep according to General Characteristics, Sleep Hygiene, Smartphone-related Factors
Of the 288 participants included in this study, 69.4% were in their 20s and 32.3% were male. 19.8% of participants did not consume caffeine at all, while 25.0% of participants consumed 300 mg or over per day. The high-risk and potential-risk groups for smartphone addiction were 67.4% and 21.5% inrespectively. 92.4% of participants used smartphones for 3 hours before bedtime (Table 1).
|
The quality of sleep in young adults varied by residence type (F=0.64, p=.020), caffeine intake (mg/day) (F=3.35, p=.019), and smartphone addiction (F=3.94, p=.021) (Table 1).
Sleep duration on weekdays was longer for unmarried than married participants (t=4.78, p=.030). People whose education level was high school or less slept longer than those with a college degree or higher (t=6.41, p=.012). Participants with jobs had shorter sleep durations on weekdays than those without a job (t=6.43, p=.021). Furthermore, sleep duration on weekdays in young adults varied by residence type (F=3.97, p=.020) and caffeine intake (F=16.82, p<.001). Unmarried participants had longer sleep durations on weekdays than those who were married (t=6.44, p=.012). According to the post hoc test, young adults living with their parents had a longer sleep duration on weekdays than those living with a spouse (p=.045). Young adults without caffeine intake had longer sleep duration on weekdays than those who consumed 1~150 mg of caffeine (p=.007), while participants who consumed 300 mg of caffeine or more had shorter sleep duration on weekdays than those who consumed 1~150 mg (p<.001) or 151~300 mg of caffeine (p=.009) (Table 1).
Sleep duration on weekends was longer for unmarried than married participants (t=6.44, p=.012). Sleep duration on weekends in young adults varied by residence type (F=3.19, p=.043) and caffeine intake (F=3.71, p=.012). According to the post hoc test, young adults living with their parents had longer sleep durations on weekends than those with spouse (p=.048). Young adults without caffeine intake had longer sleep duration on weekends than those who consumed 150~300 mg (p=.036) or 300 mg over of caffeine (p=.037) (Table 1).
2. Correlation between Sleep Hygiene, Smartphone-related Factors, Social Network, and Sleep
The average score of sleep quality in young adults was 59.34 points. The average sleep duration during weekdays was 6.86 hours, while on weekends it was 7.84 hours. The average daily sedentary duration was 7.50 hours, the subjective health status was 2.90 points, and the impact of pain over the last four weeks was 2.18 points. Characteristics of overall smartphone use was 3.26 points (range 1~5), in which convenience was the highest at 3.59 points. The young adults’ average daily smartphone usage duration was 6.19 hours. The average score of social networks in young adults was 3.26 points, with 3.07 points for family and 3.45 for friends in the subcategories. The average scores for night eating syndrome, stress level, and stress coping were 23.36, 2.93, and 71.11 points, respectively (Table 2).
|
The quality of sleep in young adults had a positive correlation with sleep duration on weekdays (r=.18, p=.002) and social networks (r=.17, p=.004) including family, which is a subcategory of social networks (r=.21, p<.001), and a negative correlation with the impact of pain over the last four weeks (r=-.29, p<.001)and night eating syndrome (r=-.38, p<.001), including sleep mood (r=-.55, p<.001) and nocturnal ingestion (r=-.21, p<.001), which are subcategories of night eating syndrome (Table 2).
Sleep duration on weekdays in young adults had a positive correlation with sleep duration on weekends (r=.50, p<.001) and sedentary duration (r=.27, p<.001), and a negative correlation with information (r=-.19, p=.002), which is characteristic of smartphone use, night eating syndrome (r=-.14, p=.016), and sleep mood (r=-.18, p=.002), which is a subcategory of night eating syndrome, stress (r=-.15, p=.012), and stress coping styles (r=-.20, p=.001). Sleep duration on weekends in young adults had a negative correlation with sleep mood (r=-.12, p=.041), which is a subcategory of night eating syndrome, and stress coping styles (r=-.12, p=.041) (Table 2).
3. Factors Influencing of Quality of Sleep in Young Adults
The factors affecting quality of sleep in young adults were analyzed with stepwise multiple regression. The variance inflation factor was less than 10, which indicates that there is no issue with multicollinearity. The factors affecting quality of sleep in young adults the most were sleep mood, which is a subcategory of night eating syndrome, impact of pain over the last four weeks, and family, which is a subcategory of social networks, with the explanatory power of 33.0% (Table 3).
|
|
DISCUSSION
|
This study consisted of a descriptive survey, examining how sleep hygiene (caffeine intake, alcohol intake, night eating syndrome, stress, and coping styles), smartphone-related factors, and social networks affect sleep in young adults aged less than 40 years.
The quality of sleep in our young adult sample was 59.34 points on average, which is below the cut-off score of 65 points, thus indicating a low quality of sleep [23]. The average sleep duration on weekdays was 6.86 hours (range: 4~12), while that on weekends was 7.84 hours (range: 4~16), both of which are lower than the recommended sleep duration on weekdays for healthy adults (7~8 hours) [7]. Our findings are lower than the average hours of sleep for Americans in their 20s (8.2 hours) and the OECD results (7.8 hours) [4, 29]. Domestic results in the OECD statistics are from 2014 and sleep duration has recently decreased. Poor quality of sleep and short sleep duration among young adults in Korea is incresed the incidence of obesity, cardiovascular disease, diabetes, and hypertension of middle-aged or elderly people [1, 2, 4, 29, 30]. Therefore, active interventions should be needed at young adults with low quality of sleep or a sleep duration of seven hours or less to prevent health problems related to sleep deprivation.
We found that the quality of sleep in young adults varied by residence type, caffeine intake, and smartphone addiction. Young adults’ sleep duration on weekdays and weekends was longer for those in their 20s than 30s, and longer for women than men. Sleep duration on weekdays and weekends was shorter for participants who were married or had jobs. Following Matricciani et al. [1], we infer that young adults with jobs tended to have shorter sleep durations due to long working hours and work-related stress, while those who were married had shorter sleep durations due to housework and child-rearing. Sleep duration on weekdays and weekends decreased as daily caffeine intake increased. Recently, young adults in Korea have been consuming an increasing amount of caffeine through coffee, tea, and other kinds of drinks, which may help in improving concentration or staying awake during the day, but causes reduced sleep duration [1, 5, 16, 31]. Health care providers should include in their interventions a appropriate daily intake of caffeine (less than 400 mg) and avoidance of excessive caffeine intake for young adults. The high-risk and potential-risk groups for smartphone addiction were 88.9%. The high risk group and the potential risk group for smartphone addiction were very high at 88.9%, which was lower than in infants and adolescents, but among adults, the smartphone addiction group was the highest [18]. Our result is similar to findings that adults who are addicted to smartphone use have reduced quality of sleep and sleep duration and experience more severe degrees of anxiety and depression [1, 5, 21]. In order to improve the sleep quality of young adults, strategies to prevent smartphone addiction are required.
When the factors affecting the quality of sleep in young adults were analyzed using stepwise multiple regression, sleep mood (a subcategory of the night-eating syndrome), the impact of pain over the last four weeks, and family (a subcategory of social networks) had the greatest impact, in that order, with an explanatory power of 33%. In young adults, Night-eating syndrome is worsened by emotional factors such as stress, which in turn causes irregular sleep patterns, thereby ultimately reducing the quality of sleep [17, 23]. In addition, physical problems such as pain and reduced health status in young adults directly affect the quality of sleep [3, 5]. Finally, young adults value social networks and are forming social networks through direct relationships and indirect resctionships by social network services or smartphone. These social relationships affect self-management such as obesity and sleep. A weak social network can cause perceived social isolation, which can negatively affect cardiovascular diseases, neuroendocrine diseases, cognitive functions, and sleep. Family in one’s social network has a greater effect than friends or local communities, on obesity-related health behaviors. Hence, it has an indirect positive effect on the quality of sleep [5, 18, 20].
|
CONCLUSION
|
The purpose of this study was to identify sleep hygiene factors affecting the quality of sleep in young adults. Factors affecting quality of sleep in young adults included sleep mood (a subcategory of night eating syndrome), the effects of pain over the last four weeks, and social networks. The above factors are similar to the factors affecting sleep in adolescents, except school life and homework. Sleep mood in night eating syndrome has been suggested as a factor affecting sleep in young adults. But the reliability of Korean Version of Night Eating Questionnaire (NEQ) is low, so there are limitations in the interpretation of the results. As young adults are an important period in forming adult lifestyles, it is suggested that occupational classifications, working hours, and work patterns that affect directly sleep, and private meetings, depression, should be added in following study. As life expectancy is increasing, it is important to focus on investigating health status for prevention rather than treating diseases. Sleep hygiene, which is crucial for one’s health, must be identified and diseases caused by sleep deprivation can be prevented through interventions design based on study findings such as ours.
|
Notes
|
This paper was supported by Konkuk University in 2018.
|
References
|
- Related articles

 KACHN
KACHN



 Cite
Cite

